HINTS Exam: Determining the Cause of Acute Vestibular Syndrome
Christie Clem, SPT
Background
During my acute care rotation at WakeMed in Raleigh I saw many patients that had been diagnosed with a stroke or vestibular pathologies. Some of the patients with vestibular signs and symptoms were initially misdiagnosed, but the vestibular evaluation done by the physical therapist gave insight that supported a different diagnosis and different medical management. Misdiagnosis could be due to practitioners not having a great understanding of the clinical presentation of various vestibular problems, not administering an exam technique correctly, not completely understanding what the exam results are meaning or not correctly identifying subtle eye movements. I was fortunate to work with a clinical instructor, Dana Thomas, MS, PT, who had completed the Susan Herdman Vestibular Rehabilitation Competency Course, in addition to, using evidence to guide her daily practice. It was during this time that I began to better understand the information that could be gathered from a bedside vestibular exam, how different vestibular pathologies can present and that some strokes can mimic peripheral vestibular problems. Acute vestibular syndrome (AVS) is a clinical condition characterized by a group of signs and symptoms: dizziness or vertigo that develops over seconds to hours and persists for at least 24 hours, nausea/vomiting, nystagmus, head motion intolerance and gait instability.1 AVS can be caused by a peripheral or central pathology, but can have the same presentation no matter the cause. It was with these patients that I learned the HINTS exam, a three-part bedside oculomotor exam, can be used to differentiate between a peripheral and central cause of AVS.1,2
If it were not for this rotation, I would not have been introduced to the HINTS exam or have realized how valuable physical therapists can be in helping to diagnosis vestibular pathologies in an acute setting. I also witnessed my CI use evidence based research to educate others (PTs, physicians, physician assistants) in how to perform vestibular tests and interpret the results including the HINTS. This rotation increased my interest in vestibular pathologies, clinical presentations and exam techniques. I decided to make this topic the focus of my literature review during my 3rd year of the PT program with the goal of presenting the information to other UNC PT students.
The Project
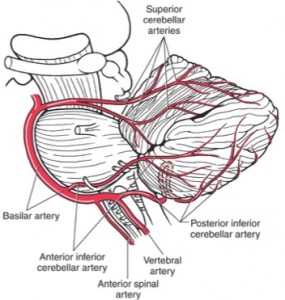
During the Evidence Based Practice II course, I began gathering research related to the PICO question, “in a 70 year old man with acute vestibular syndrome, is a clinical bedside exam or MRI more accurate in determining if the cause is central or peripheral?” The information gathered was used to create a critically appraised topic that concluded the HINTS exam is better at ruling out a stroke than MRI performed within 48 hours of symptom onset. The following semester I gathered additional information about the specific arteries of the brain’s posterior circulation that cause AVS, vestibular rehabilitation and identified new studies that included the HINTS exam. I created a VoiceThread presentation and presentation handout from the information I gathered. The eDPT and tDPT students in the PHYT 885 Advanced Neuromuscular Intervention course were selected to be the audience for the presentation materials. The main goal of the presentation was to make PT students aware that a dangerous cause of AVS, such as a stroke, can have the same clinical presentation as a benign peripheral cause of AVS. The specific learning objectives included being able to recognize the clinical presentation of AVS, describe the 3 components of the HINTS exam and interpret the results of the HINTS exam to determine if the cause is central or peripheral.
Reflection
Those that viewed the presentation were asked to complete a 10-question pre- and post-test assessment and a presentation feedback form. The pre- and post- assessments allowed me to evaluate if the learning objectives had been met. The pre-test average was 50% while the post-test average improved to 80%. There was only one question that every person answered correctly in the pre-test assessment, where as seven of the questions were answered correctly by everyone on the post-test assessment. Overall, the presentation feedback was positive. The average rating for each question ranged from 4.33 to 5 on a 5-point scale. The highest ratings were for the information being of important clinical relevance, a thorough explanation of the content and that the included videos enhanced understanding. Some changes have already been made to the VoiceThread based on the questions that were consistently missed on the post-test assessment. I also plan to update the handout based on feedback in order to make it more beneficial and user friendly.
Acknowledgement
It would not have been possible for me to complete this project without the support of my Capstone committee members. I would like to thank Dana Thomas, my CI at WakeMed, for helping me gain a better understanding of vestibular anatomy, vestibular examination techniques and how to interpret the results. She modeled how to be an evidence-based practitioner while stressing the importance of not making the patient fit the diagnosis you have in mind, but to instead “let the exam speak for itself.” In addition to the eight weeks of guidance Dana provided as a CI, she also provided valuable insight and feedback throughout this project. I would also like to thank Dr. Karen McCulloch for her assistance throughout this process. I appreciate the feedback while creating the materials, her willingness to allow the students in her PHYT 885 class to be the intended audience this year and suggesting it be viewed in upcoming years by PT students before going on their acute clinical rotation. Finally, I would like to thank Gabrielle Scronce, PT for taking time out of her busy schedule to provide valuable feedback on the presentation and handout. Gabrielle was able to give useful feedback from the prospective of a recent UNC PT graduate that was not familiar with HINTS exam.
Materials Associated with this Project
HINTS Exam Pre-Test: 10 Questions (link to SurveyMonkey; PDF version is above)
HINTS Exam VoiceThread (32 min)
HINTS Exam Post-Test: 10 Questions (link to SurveyMonkey; PDF version is above)
HINTS Exam Presentation Feedback (link to SurveyMonkey; PDF version is above)
Resources
- Kattah JC, Talkad A V, Wang DZ, Hsieh Y-H, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009;40(11):3504-3510. doi:10.1161/STROKEAHA.109.551234.
- Tarnutzer A a., Berkowitz AL, Robinson K a., Hsieh YH, Newman-Toker DE. Does my dizzy patient have a stroke? A systematic review of bedside diagnosis in acute vestibular syndrome. Cmaj. 2011;183(9):571-592. doi:10.1503/cmaj.100174.
- http://clipart.me/free-vector/dizzy [picture]
- http://clinicalgate.com/the-cerebellum [picture]


10 Responses to “HINTS Exam: Determining the Cause of Acute Vestibular Syndrome”
Gabrielle Scronce
Christie,
This is such a well-done project! I learned a great deal from your capstone that is important to know for the work I do. Thank you for your hard work in making this information accessible!
Gabrielle
Debbie Thorpe
Hi Christie
You did a great job with your capstone project!! I really enjoyed listening to the voicethread presentation. You have created a great resourse for future 2nd and 3rd year students for use on clinical rotations. Your presentation was informative, well paced and organized. Your slides were very interesting and informative. Very professional product!!! Good luck on your clinicals this summer!!
Best
Debbie
Chelsea Parker
Hi Christie,
I really enjoyed the handout and voicethread! I got TONS of good experience working with BPPV in a rural outpatient clinic on my last rotation. My CI had a handout of tests to perform that was almost an entire page long! The HINTS exam seems like a much more realistic way to determine whether it is a central or peripheral pathology. Most patients that I saw in the clinic presented with AVS, so I would believe this is still relevant, though I am seeing them quite a few days after onset.
I have already printed out the hand-out and can’t wait to put it to use in the future! Thanks so much for the valuable information!
KMac
Nice job on this project, Christie – As you reflected earlier in your response to Rob, this assessment is very specific to the acute vestibular presentation with duration that is inconsistent with the typical durations we associate with some of the other clinical syndromes that PTs treat. As Christie and I have discussed, we feel this module is most appropriately shared with 2nd or 3rd year students who are planning to do an acute rotation (so they already have a foundation of vestibular knowledge to add this to). Dana even said in my interactions with her that she doesn’t think this is a widely used approach (but presumably will increase over time – perhaps b/c of Christie’s project!).
kmac
Sarah Morrison
Hi Christie,
I really enjoyed your presentation and handout! I will definitely keep the handout for clinical use. I worked with many, many patients in outpatient at Fort Bragg after TBI and performed the HINTS tests, along with a battery of other vestibular and visual tests, without even realizing I was following this protocol! I had no idea of the high sensitivity of those specific tests for individuals with stroke. I’d be interested to know about the accuracy of the test for patients with TBI since focusing on just a few tests could help differentiate between central and peripheral dysfunction in a lot of the military service members I saw, and maybe then help the PT’s provide more effective treatment. Thank you for sharing and great job!!
Abbie Marrale
I worked with a number of patients suffering from vestibular disorders in the outpatient neuro setting, however I had never heard of AVS. The information you were able to bring together was easy to follow and comprehensive. Furthermore, I was able to see how far my learning on AVS had come from taking the pre- and post-tests.
It is very helpful to have knowledge of this important syndrome, especially its connection with posterior stroke.
One thing this presentation made me think of, was in the outpatient setting we had a number of patients who had been diagnosed with BPPV in the hospital (following a stroke), and sent for further PT after discharge. I don’t remember seeing a HINTS exam performed, or seeing any information regarding AVS. Just curious how often this condition could be missed, and if it would be something that outpatient PTs may encounter as well.
Christopher Hope
Hi Christie. Excellent work all around. The pre- to post-test improvement doesn’t surprise me at all since you did a fantastic job presenting the HINTS exam and explaining the material. I wasn’t familiar with the exam procedure prior to your presentation, so thanks for sharing such a useful tool.
Your presentation was entertaining, informative, and interesting. It was very easy to follow along since the pace was perfect and the narration was clear and comfortable. The slides were succinct enough to maintain attention while providing enough information to be educational, all of which complimented the narration. The videos were particularly helpful in allowing visual application of the written and spoken information. Great job on the presentation.
I also enjoyed the handout and will keep it as a reference for future clinical practice. The chart makes for a quick and easy reference guide, while the information on the other pages helps to add depth. Again, great job.
You pointed out that your CAT concluded that the HINTS exam is better than MRI at ruling out stroke in the first 48 hours of symptoms. That leads me to a couple of questions: (1) What is the current standard diagnostic protocol for someone presenting to an ER with AVS? Is the first response to order an MRI, or are there other diagnostic and/or neurological tests performed? (2) Finally, did you come across any literature that indicated if any one provider (i.e. neurologist, physical therapist, etc) is better at administering and interpreting the HINTS exam compared to other providers? Are PTs performing this exam more often than physicians or PAs? Thanks for clarifying.
Again, impressive work. Kudos for the work you’ve put into it. You did a really great job.
– Chris
Christie Clem
Rob,
Thanks for taking the time to review my project. I hope you found the information beneficial and maybe on your upcoming clinical you will have a chance to use some of these oculomotor exams.
I will now try to answer your question. I did not come across a specific number for how the HINTS compares to MRI performed more than 48 hours after the onset of acute vestibular syndrome. In the study by Kattah et al (2009),1 8 of the 69 (12%) patients with an ischemic stoke in the posterior circulation had a falsely negative MRI within 8 to 48 hours of symptom onset. When these patients had a follow-up MRI an average of 3 days later (ranging from 2 – 10 days) all of the ischemic strokes were then visible on imaging. The study did not say if these patients still had AVS at the time of the follow-up MRI and it did not say if the HINTS exam was performed again if the patient still had AVS.
The HINTS should only be used for patients that currently have AVS. The clinical symptoms must have been present for at least 24 hours, but there is no exact time frame for how long the signs/symptoms will last. Once AVS is no longer present, it would not be possible to compare the diagnostic accuracy of imaging to the bedside exam.
I did not read this in any literature, but Dana Thomas, my committee member that uses the HINTS a lot at WakeMed, said multiple radiologist have told her that some strokes are too small to ever show up on MRI or MRA. Dana believes this has been the case with some of her patients. These patients had AVS and a central HINTS exam, but nothing showed on their MRI (even after 48 hours). The radiologist reported the findings as no confirmed pathology on the visible vessels, but was unable to make any statements about the vessels that were too small to be seen.
I hope this begins to answer your question. If I come across a more specific answer I’ll let you know.
Christie
Rob Sykes
Phenomenal job, Christie! Not to repeat what Kelly has already said, but your VoiceThread presentation and handout are really well done and easy to follow. I am excited to put this information into practice. I do have one question. I understand that the HINTS exam is more sensitive than MRI within the first 48 hours of symptom onset. Do you know how the HINTS exam compares to MRI that is performed beyond the the first 48 hours of symptom onset?
Kelly Hewitt
Hi Christie,
I have only encountered a couple of patients with vestibular conditions while on clinical, but shadowed in a balance and vestibular clinic before PT school. It is definitely a very interesting area and one that PT can significantly influence. I really liked the set-up of your capstone and think the materials are clear and helpful! (I downloaded and saved your HINTS exam overview document) I can tell that you used to be a teacher, because everything is so clear and straightforward. Thank you for sharing this knowledge and your creative teaching materials!