Pusher Syndrome Post-Stroke:
Background Information, Patient Presentation, and Evidence-Based Intervention Strategies
Created by Hannah Leshin
Background Information
Pusher Syndrome (PS) is an impairment that occurs following a stroke, affecting patients’ perception of postural vertical.1 The patient presentation of PS is categorized by (1) “spontaneous body posture” leaning to side contralateral to the lesion; (2) abduction and extension of the extremities ipsilateral to the lesion; and (3) resistance to passive correction of posture.2 Occurring in between 10-16% of patients with stroke, PS results in postural instability and increased risk of falls.3,2 PS does not impact long-term functional potential, but often slows the course of recovery for patients with stroke.4
Project Overview
On my clinical rotation in inpatient rehabilitation at Wake Forest Baptist Medical Center in Winston-Salem, NC, I treated several patients with PS. Although the Neuromuscular I course introduced this impairment, I was not aware of evidence-based interventions specific to PS. My clinical instructor at the time, Lauren Suggs Boyd, DPT, encouraged me to explore this topic in as a potential subject for my Capstone project.
In EBP II, I focused my literature search on the following PICO question: In elderly patients 1-2 weeks post-stroke with Pusher Syndrome, is visual feedback therapy more effective than body weight supported (BWS) ambulation in reducing pushing through the uninvolved side? Despite scant intervention-based research regarding BWS for PS, I was able to gather some high-quality evidence that examined visual feedback, computer-based feedback, and assisted gait training.5,6 I performed an in-depth review of the highest quality evidence available in creation of my Clinically Appraised Topic (CAT).
I used the evidence from the CAT as a foundation for my Capstone. The goal of this project was to create several resources for entry-level DPT students to access during the Neuromuscular I course and on future clinical rotations to improve students’ ability to assess and treat patients with PS.
Capstone Products
Over the course of the UNC DPT curriculum, I have benefitted from many different teaching tools and styles. In order to best serve the students, I created 3 educational products about PS:
- A VoiceThread presentation that details information about patient presentation, theoretical concepts, and intervention strategies
- Click here for a PDF version of this powerpoint. Due to the large size of the file, I had to compress the images for upload, which reduced the quality of the images. Students can download the original PDF through Sakai.
- A reference document highlighting key points from the presentation
- An evidence table describing intervention-based research about PS
Improving the Student VoiceThread Experience
My ideal setting for this presentation would be an in-person lecture to students. However, since the Neuromuscular I course is taught in the fall semester, I created a VoiceThread for future classes. In my time as a UNC DPT student, I have watched my fair share of VoiceThread presentations. I understand it can be difficult to keep attention to the lecture, take thorough notes, and digest all of the material. In an effort to avoid “death by powerpoint,” I used several tactics:
- I provided a supplemental reference document to allow students to pay full attention to the presentation without being distracted by note-taking.
- I included a built-in break for the VoiceThread. In my 3rd year, I struggled to allot myself a break during these presentations since I would watch in the comfort of my home. Encouraging breaks may help to prevent mind wanderings and mental fatigue.
- I included tips from “Making Better PowerPoint Presentations” from the Vanderbilt University Center for Teaching, including:7
- Bulleted lists on slide
- Simple Powerpoint color/theme
- Reduced text on slide
- Inclusion of graphics with verbal explanation
- Provided PDF version of slides
- Like some of my favorite lecturers in the UNC DPT program, I also included a few pictures of my life to give some levity to the presentation and allow more of my personality to come through for future students.
Evaluation
In order to ensure that the entry-level DPT student would understand my project, I recruited several of my classmates to perform peer reviews of all of my capstone materials with a lens towards health literacy. Classmates Will Harrison, Molly Miller, and Chloe Smith assisted in this review, representing students with a wide variety of physical therapy interests. I also received feedback from my Capstone committee throughout the creation of these educational materials.
Second year DPT students in the Neuromuscular I course will view the materials. This course is not offered in the spring semester, so no feedback from this audience is currently available. However, I have created a survey for students to test content understanding and provide feedback in the future. Students have the option of “free text” to provide feedback regarding strengths and areas of improvement for this presentation.
Acknowledgments
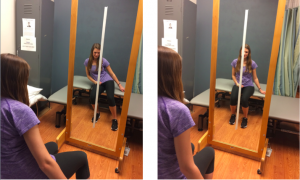
I would like to thank my Capstone advisor, Karen McCulloch, PT, PhD, NCS, for her feedback, guidance, and patience as I enter the teaching realm with this project. Thanks to my Capstone committee members Vicki Mercer, PT, PhD, and Dr. Boyd for their input and encouragement. The presentation would not have been complete without the help of Mary Beth Osborne, PT, DPT, NCS, who connected me with a fantastic patient to film for the VoiceThread. Thanks to Dr. Osborne’s Duke University DPT students Kelly Mullahy, Aubrey Burnside, Brittany Butler, and Callie Beasley who allowed me to include them in my presentation! A final and hearty thanks to my wonderful peers for evaluating and contributing to this project. Will, Chloe, and Molly gave me excellent tips for improving the presentation. Kenzie Owens and Kristen Ignaszewski were willing and wonderful patient/therapist models. I am proud to be a member of the UNC DPT Class of 2017!
References
- Karnath HO, Ferber S, Dichgans J. The origin of contraversive pushing: evidence for a second graviceptive system in humans. Neurology. 2000;55(9):1298-1304. http://www.ncbi.nlm.nih.gov/pubmed/11087771. Accessed October 10, 2016.
- Karnath H-O, Broetz D. Understanding and treating “Pusher Syndrome.” Phys Ther. 2003;83(12):1119-1125. doi:10.1016/s0003-9993(96)90215-4.
- Gandolfi M, Geroin C, Ferrari F, et al. Rehabilitation procedures in the management of postural orientation deficits in patients with poststroke pusher behavior: a pilot study. Minerva Med. 2016;107(6):353-362. http://www.ncbi.nlm.nih.gov/pubmed/27635603. Accessed February 16, 2017.
- Pedersen PM, Wandel A, Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS. Ipsilateral Pushing in Stroke: Incidence, Relation to Neuropsychological Symptoms, and Impact on Rehabilitation. The Copenhagen Stroke Study. Arch Phys Med Rehabil. 1996;77:25-28. http://ac.els-cdn.com/S0003999396902154/1-s2.0-S0003999396902154-main.pdf?_tid=24f75258-1a31-11e7-b442-00000aacb35d&acdnat=1491418583_2333a39f2c881003bd25db45b6c464a3. Accessed February 17, 2017.
- Yang Y-R, Chen Y-H, Chang H-C, Chan R-C, Wei S-H, Wang R-Y. Effects of interactive visual feedback training on post-stroke pusher syndrome: a pilot randomized controlled study. Clin Rehabil. 2015;29(10):987-993. doi:10.1177/0269215514564898.
- Krewer C, Rieß K, Bergmann J, Müller F, Jahn K, Koenig E. Immediate effectiveness of single-session therapeutic interventions in pusher behaviour. Gait Posture. 2013;37(2):246-250. doi:10.1016/j.gaitpost.2012.07.014.
- Making Better PowerPoint Presentations. Cent Teaching, Vanderbilt Univ. 2017. https://cft.vanderbilt.edu/guides-sub-pages/making-better-powerpoint-presentations/. Accessed April 4, 2017.

17 Responses to “Pusher Syndrome Post-Stroke”
Mary Runey
Hannah,
I just wanted to say nice job on all of your materials. This topic is very interesting and your project has been very informative. As many have stated, you did a great job at being thorough throughout the project. The outcome measures were new to me to think about for this populaiton. During your IPR clinical how often did you feel like you saw this population? I did not do an IPR clinical and I cannot say I have encountered many patients with PS. But I know some students have and I think that this voicethread will be a great addition to the curriculum. Thanks again for choosing this topic and allowing us to further understand Pushers Syndrome.
Lauren Boyd
Hannah,
Well done on all of your materials! I agree with Will that you did a great job being thorough, yet concise on a topic that is very narrow in scope. Thank you for helping me remember my neuroanatomy, introducing me to different outcome measures specific to this population, and providing simple, but great treatment ideas with pictures! Your materials really do appeal to all learning styles.
It was such a pleasure getting to work with you in the clinic with several patients with PS and it makes me smile to now see you teaching others about what you have learned! Kudos to you! Keep up the good work and finish strong!
Megan Schilter
Hannah-
I am so impressed with your work and the voice thread was excellent–you have a really warm and focused manner of speaking that made learning this content enjoyable. I wish I had this module last year during neuro, especially since I ended up encountering many patients with pusher syndrome during my patient rotation. I am also quite impressed by the resources you used to improve the presentation itself, rather than just the content. It is clear that you assessed how learners would respond to the voice thread, not just what information you could include.
Will you be presenting this material again? I think it would be a great resource for physical therapists practicing in a variety of settings and could serve as a great refresher for practicing clinicians.
Congratulations on a job well-done. Best of luck on this upcoming rotation 🙂
Mary Beth Osborne
Beautifully done, Hannah! Your CAT was very well done (sure glad I’m not grading those anymore :)) and the voice thread turned out great! Mr. B loves the limelight, so happy he was able to help you out.
Wishing you the very best during clinicals and graduation will be here before you know it! Mary Beth
Kristen Ignaszewski
Hannah,
I’m glad I could be a part of your capstone project! Wonderful job with the presentation of the materials you created. I know future DPT students will really benefit from the VoiceThread presentation you created, with focus on avoiding “death by PowerPoint”. I also really appreciate the quick reference guide you created, and know this will be the first place I look if I ever encounter a patient with PS after a stroke! Congratulations, and great work on your capstone project!!
Terra D Osmon
Hannah,
You did a fantastic job! Specifically, I really like how your capstone is comprehensive of the topic of pushers syndrome and you did a wonderful job of making it easy to understand. I like that you had breadth on the topic just enough depth for with respect to pertinent key details on all the key topics with respect to the issue, what to expect, the anatomy, outcome measures, and treatments. I appreciate that you developed a resource guide and I think this will greatly benefit me when I go on my last clinical rotation in acute inpatient rehab as I will be working primarily with stroke patients. This is going to be so helpful and I am going to save it so I can review before starting. Thank you so much for your contribution and all the hard work!
Hannah Leshin
Terra, thank you for the kind comments! I am happy to hear that my presentation improved your understanding of a unique patient population. Please let me know if you treat any patients with PS on your rotation and if/how these materials improved your treatment POC.
KMac
Hey Hannah, We have started teaching the bucket test in 784 when we do vestibular lab, I’m not sure that Vicki knows this 🙂
The project looks awesome, I still need to listen to the voicethread, but I’m happy that we’ll have this as a resource for 784 now! Thanks for all your hard work, and I’m glad that the pt with Mary Beth worked out.
kmac
Hannah Leshin
KMac, it’s so cool that you are now doing the bucket test in lab! I watched several Youtube videos about the test, but have not seen the test performed in clinic. Maybe on my last rotation in OP neuro? Who knows! There may be a few tweaks to make before the VT is posted for 784, but I am really proud of the materials. Thanks again for all of your guidance throughout this process.
Will Harrison
Hi Hannah!
You did an awesome job on your capstone project! One thing that I really love about your project is how narrow in scope it is, because it allows you to go very in-depth on one particular topic that we will almost inevitably encounter if we work with patients with stroke. From my experiences in both the acute care setting and the inpatient rehabilitation setting, I have worked with several patients with PS. I have continually struggled to effectively treat these patients, so your presentation has been especially helpful to me. Your VoiceThread was excellently done in all aspects (great slides, very nice narration, and good pacing), but my favorite part is the Reference Handout. Honestly, the handout is something that I will print off and take with me to my next clinical rotation this summer (inpatient rehabilitation in Charlotte, NC). The handout is short, to the point, and provides great practical treatment options. I definitely think that your capstone will be successful in accomplishing your goal of adding value to the Neuromuscular I Course. Your explanation of the patient’s incorrect body position due to the misperception of vertical, along with the anatomical descriptions provide great insight into this particular deficit. Great job!
Thanks,
Will
Hannah Leshin
Will, thanks for your feedback! I have to say thank you once again for being a fantastic peer reviewer. You were on point with all of your suggestions. I am glad that you appreciate the depth of my presentation. This can be a complex topic to understand, so I wanted to devote sufficient time for explanation of the deficit itself, in addition to treatment strategies.
My idea for the resource guide is exactly as you indicate, printing it off and having it available while on rotation in the IPR setting. In fact, I emailed the current 2nd year students a link to the presentation in the event they begin treating a patient with PS. If you do treat any patients with PS on your last rotation, please let me know how/if the resources helped you improve your treatment strategies and goals.
Meredith Smythe
Dear Hannah,
I had the pleasure of looking over your capstone materials. Your voicethread was enjoyable and logically organized. I really enjoyed the incorporation of example pictures and the videos of the patient case. This helped my comprehension and made the voicethread effective. I also enjoyed the personal touches that you included. It was helpful for me that you included a neuroanatomy slide to review certain structures. I appreciated having a copy of the slides so that I could follow along with the presentation and take notes. You did a very good job at speaking clearly and at a reasonable pace. I think that by listening to this presentation a physical therapy student could achieve all the learning objectives that you listed.
Your hand out was nicely organized and clear. You included a very good explanation of PS presentation and etiology. I liked that you included both descriptions of the outcome measures and references to access them. You also included clear treatment options with many examples.
The evidence table was well organized, nicely presented and you provided a clear description of each study. It was interesting that the visual Wii balance feedback program showed an advantage over the traditional visual feedback group in the first study. I wanted to know a bit more about the weaknesses and limitations of the studies. Since many of these studies were small pilot trials do you think that given the evidence there should be larger randomized controlled trials conducted?
How would you treat pusher syndrome when a person is also experiencing unilateral neglect? It seems that many of the external cues are visual due to the patient’s intact subjective visual vertical. Thank you for preparing such a high quality project. Great job.
Meredith Smythe
Hannah Leshin
Meredith,
Thank you for reviewing my Capstone and for providing thoughtful feedback! I am glad that the neuroanatomy slides were additive to the lecture, as I spent a lot of time researching and reading materials in order to consolidate that information in a clear, informative way. I have struggled with the quality of evidence available since I began my literature searches in EBP II. I absolutely think that there need to be more randomized controlled trials for this patient population with regard to intervention strategies. Since I submitted my CAT, there has been 1 new RCT published, which shows promise for research about this population. I did review this new article and include information on the handout and VoiceThread to made the information as up-to-date as possible. Here is the citation for the newest literature:
Gandolfi M, Geroin C, Ferrari F, et al. Rehabilitation procedures in the management of postural orientation deficits in patients with poststroke pusher behavior: a pilot study. Minerva Med. 2016;107(6):353-362. http://www.ncbi.nlm.nih.gov/pubmed/27635603. Accessed February 16, 2017.
For a patient with unilateral spatial neglect (USN), you would need to integrate principles of treating pusher syndrome with principles of USN. For example, positioning yourself and speaking to the patient on the patient’s involved side remains important, while still encouraging weight shifting towards the pushing side. This might require the assistance of a PTA or co-treatment with OT to be most effective.
I hope that answers all questions. Feel free to contact me with any others!
Best,
Hannah
Vicki Mercer
Hi Hannah!
Great job on this project! I think the materials you have created will be very helpful for students in PHYT 784. Have you ever seen anyone do the bucket test that you describe in the VoiceThread?
Vicki
Hannah Leshin
Vicki, I have not seen the bucket test performed in clinic. I did watch several videos on YouTube to get a sense of the test being performed, and I read up on the reliability for in-clinic use. KMac suggested that I include the test in my discussion of SVV. I think it’s great that you have included it in PHYT-784 lab!
Mackenzie Owens
Hi Hannah,
Thank you for providing these helpful resources on Pusher Syndrome! I think your capstone project will be a valuable addition to the Neuromuscular I course and to our class as well as many of us have our last rotation in the neuro setting. I appreciated how you reflected on your learning experiences with VoiceThread presentations in the past and made changes to benefit future students including the provision of a reference document and a built-in break. I felt that the VoiceThread learning objectives were well outlined and the recording was clear. I also enjoyed that the VoiceThread integrated your patient experiences. The picture demonstrations of postures, inclusion of safe guarding techniques, discussion of verbal and somatosensory cues, and application of this information to a patient example will all be helpful to review before returning to the clinic setting. Finally, I thought it was a great idea to include classmates with various interests in the evaluation of this project and to seek “free text” feedback from future students electronically. I am excited to utilize these resources for my upcoming clinical rotation in inpatient rehab!
Thanks,
Kenzie
Hannah Leshin
Kenzie, thank you for taking the time to review my Capstone. Thanks also for being a fantastic (and willing) model! As my roommate during my IPR rotation, you saw first hand my frustration in treating this patient population. I am glad that including my own experiences in the VoiceThread was beneficial to your learning experience. Please let me know if you treat a patient with PS on your last rotation, and if these materials improved your confidence in implementing an effecting POC!