Progressive Return to Activity for Service Members with Acute Mild Traumatic Brain Injury
By: Caroline Cleveland, SPT
Background
In January 2013, while I was active duty in the Army, I began my prerequisite physical therapy observation hours in the Intensive Care Unit at Landstuhl Regional Medical Center in Germany. The first patient I saw on my first day at Landstuhl was my friend from college and the Reserved Officer Training Corps, whose helicopter had crashed in Afghanistan. I recognized his wife at his door, but I barely recognized him on the hospital bed. He was in a coma, had just had a decompressive craniectomy, and was still struggling through cardiac pulmonary edema. Both his legs and multiple ribs were broken, and, as his mother broke down in my arms, I wondered if I could handle the emotional memories of my own deployment that were provoked by seeing such pain and suffering. However, in remembering my deployment, I recalled my explosive ordinance disposal specialist who had been shot in the head – his brain grazed by the bullet – and the video his wife sent of him walking six months later with the facilitation of his physical therapist. I held my friend’s swollen hand there in Landstuhl, and I reaffirmed my commitment to serve people and families touched by injury and disability such as traumatic brain injury (TBI).
While the two aforementioned men initially inspired my passion for TBI rehabilitation, it has been the leadership and mentorship of two women that has continued to empower my contributions to this field of study and clinical application. After I separated from the Army, Dr. Karen “Kmac” McCulloch graciously took a chance on me by hiring me onto her Assessment of Military Multitask Performance study, which investigated the validity of a post-concussion/mild TBI return-to-duty test battery. Observing firsthand the challenging effects of mild TBI on fifty participating service members, while working with and learning from Kmac and her research coordinator, Dr. Amy Cecchini, I gained a greater understanding of concussion research and rehabilitation. Concurrently, both women encouraged and supported me as I took my final prerequisites and applied to physical therapy school.
Once in school, I maintained a focus on concussion through collaborating on a publication with Kmac and Amy, through POWAR-TOTAL: Portable Warrior Test of Tactical Agility pilot testing, and through coursework such as my critically appraised topic on rest versus activity post-concussion. When I was accepted to Walter Reed National Military Medical Center (WRNMMC) for my final clinical rotation, I began shaping a capstone project that would benefit Walter Reed rehabilitation staff and patients, as well as contribute to Kmac and Amy’s continued research efforts surrounding post-concussion care.
Overview
TBIs are categorized as severe, moderate, and mild. Of the 18,311 TBIs sustained among U.S. military service members (SM) in 2017, 1% were severe, 14% were moderate, and 85% were mild.1 These categories are distinguishable based on loss of consciousness, altered mental status, and post traumatic amnesia (PTA). For instance, a TBI is categorized as mild if the SM loses consciousness for up to 30 minutes, demonstrates a disoriented state for less than 24 hours, or experiences PTA for less than 24 hours. 15% of SMs sustain at least one mild TBI during their military career,2 and early intervention of concussions that do not resolve after 24 hours of rest is critical to prevent prolonged disability and the potentially compounding effects of multiple TBIs.
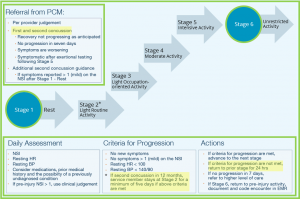
Progressive Return to Activity (PRA) evolved from gaps in previous military post-concussion guidance, and it is the current standard of care for service members within 24 hours of an acute concussion.3 PRA is a six stage progression of activities in physical, cognitive, and balance domains used to return service members to their pre-injury level of symptom resolution.3 Since PRA includes separate guidance for primary care managers and rehabilitation providers, this project aimed to outline the nuanced relationship between the two sets of guidance, specifically geared toward informing the rehabilitation provider’s understanding. The project’s literature review provides a more thorough description of PRA’s evolution, implementation, and way forward.
Statement of Need
As the nature of military operations makes it impossible to prevent all concussions, early diagnosis, targeted primary care treatment and, when needed, rehabilitation services may serve as a form of prevention by minimizing the potential for the compounding effects of multiple concussions. Thus, awareness and implementation of current evidence-based PRA clinical practice guidelines are paramount to intervene against the mitigatable burdens that may impact the service member, the mission, their unit, and their family.
As a DoD affiliate and the leading institution for military rehabilitation, Walter Reed National Military Medical Center WRNMMC represents a vital hub for PRA implementation within the military medical community. Although the overall incidence of mTBI has declined in recent years, advanced screening techniques enable more accurate and earlier diagnosis. With the still significantly high numbers of SMs with mTBI, the PRA principles remain applicable to rehabilitation providers, and ongoing clinical education remains a critical tool to ensure implementation of current evidence based practice in the midst of staff turnover.
This WRNMMC educational intervention is also intended to contribute to Dr. McCulloch and Dr. Cecchnini’s larger ongoing study examining the use of education to influence primary care provider’s PRA knowledge and implementation. By collecting rehabilitation providers’ data via a feedback form relevant to their knowledge and current practice prior to in-servicing and their knowledge and anticipated practice after in-servicing, this project seeks to determine the effectiveness of education in influencing PRA implementation. In this way, this project and the promotion of the PRA resources may also contribute to larger TBI efforts relevant to both military and civilian populations.
Products
Products created for this project are as follows:
Feedback: Evaluation and Survey Form
Additional PRA resources published by Defense Veterans Brain Injury Center and cited in this project are freely available at dvbic.dcoe.mil.
Evaluation
The goals of the project’s rehabilitation provider presentation at WRNMMC include that staff successfully (1) identify the founding principles of PRA, (2) identify patients who are appropriate for PRA, (3) appropriately apply PRA guidelines to progress patients through the rehabilitative process, (4) identify available resources to further guide employment of PRA in clinical practice, and (5) share honest feedback on actual practice previous to in-servicing and anticipated changes to clinical practice following in-servicing. The attainment of these goals, as well as general recommends for the project, will be collected from the target audience after the presentation via the feedback form.
Self-Assessment
My personal learning objectives for this project were to refine my clinical knowledge in evidence-based neuro-rehabilitation, specifically PRA, and practice my general teaching and public speaking skills to identify areas for future improvement. These learning objectives nest with my professional development goals to (1) serve as a physical therapist in a setting that screens for and treats patients with mild TBI; (2) serve as an educator on TBI awareness, prevention, and intervention; (3) serve as a collaborator in military-civilian mild TBI research.
Upon reflection, this project has enlightened my understanding of PRA, as well as deepened my understanding of the complexity of concussion treatment and the evolving body of research that informs treatment. While PRA is not recommended for service members whose concussion is over 24 hours old, the limitation of its use amongst high incidences of chronic concussion in the military does not discourage me so much as it enthuses me to advocate for screening and early intervention. Additionally, I think some concepts of PRA may be useful in rehabilitating chronic concussion, such as conducting exertional testing to establish sub-symptomatic thresholds from which to gradually progress activity and return-to-duty.
Certainly, I always want to do something bigger for the betterment of my patients, my community, and our society at large. However, that sentiment tends to paralyze me more than drive me; thus, I have come to realize that it is better to do something within my sphere of influence than it is to just ponder how I might save the world. I am honored to have the opportunity to serve my brothers- and sisters-in-arms at WRMMC, and I am equally grateful to be able to present my project there. I hope this project will be another worthy step in benefiting the military medical community, as well as my own patients through the knowledge I have gained. Indeed, our greatest impacts often occur through our interactions with one person at a time. Of the many people who have impacted my life, one of them will be at WRNMMC: my friend whose hand I held over five years ago at Landstuhl, not knowing whether he would live or die. I am happy to share that he is very much alive, and he is a continual reminder of why even the smallest efforts toward expanding and improving TBI care matters!
Acknowledgments
First and foremost, I would like to thank my family, who have unconditionally supported me prior to and through this doctor of physical therapy program. This includes Kmac and Amy, who have become like family to me, gifted me with their professional examples and personal wisdoms, and empowered me to actualize so many of my aspirations – including this project – over the past five years. To Kmac and Amy – thank you for not just all that you have done for me but also for all that you do to serve and care for my brothers- and sisters-in-arms by spearheading TBI research and education.
I would also like to acknowledge COL(R) Dr. Mary Kay Hannah and Dr. Dana McCarthy who made it possible for me to fulfill my final clinical rotation at WRNMMC, as well as Dr. Wendy Giles and Dr. Karen Alberding for affording me the opportunity to present this project to WRNMMC rehabilitation staff.
References
1 Defense Veterans Brain Injury Center. DoD Worldwide Numbers for TBI Worldwide Totals. 2017.
2 Chapman J, Diaz-Arrastia R. Military traumatic brain injury: a review. Alzheimer’s and Dementia. 2014;10:S97-S104.
3 DVBIC & DCoE for Psychological Health and Traumatic Brain Injury. Progressive Return to Activity Following Acute Concussion/Mild Traumatic Brain Injury: Guidance for the Rehabilitation Provider in Deployed and Non-deployed Settings. DCoE Clinical Recommendation, 2014.
Image #1 retrieved from: https://thedisorderofthings.com/2012/02/19/all-your-brain-are-belong-to-us/
Image #2 adapted from: DVBIC & DCoE for Psychological Health and Traumatic Brain Injury. Progressive Return to Activity Following Acute Concussion/Mild Traumatic Brain Injury: Guidance for the Rehabilitation Provider in Deployed and Non-deployed Settings. DCoE Clinical Recommendation, 2014.

4 Responses to “Progressive Return to Activity for Service Members with Acute Mild Traumatic Brain Injury”
Caroline Cleveland
Kristin, the statistics are indeed startling and really highlight the importance of continued concussion research and education. Even before deployments started slowing down, the military’s route clearance and explosive ordinance disposal technology and training began mitigating some of the more severe blast-induced TBIs. Yet, Airborne operations (parachuting out of planes), Air Assault operations (rappelling out of helicopters), and general rappelling and obstacle course training have remained a constant contributor to falls and mild TBIs. Thanks for checking out my project, and I’m glad you appreciated it!
Caroline Cleveland
Thank you, Kmac! I am looking forward to seeing you at Walter Reed as well; let the adventures continue!
Kristin Wrigth
Caroline! What a great project you put together. I am surprised that the percentage of severe TBI’s is as low as it is. I’m not sure why this surprises me but I guess because of the environment and force of some blasts I would think there would be more severe TBI’s. However, the residual effects of a mTBI can be life changing and it is great to have a plan of action in place to get the SM’s back on their feet. I like how you incorporated scenarios at the end of the presentation to make it more interactive. I think this will be a great resource for your next clinical rotation! Great work!
K-Mac
Love this project, Caroline – and I’m excited that I’ll get to see you in clinic at WRAMC!!! Looking forward to that in many ways, to learn more about what is happening there and to inform possible PRA revisions for the future. You did a great job of tracking on this autonomously and modifying it as is appropriate for the audience. I’ll look forward to hearing what the therapists there have to say about it.
kmac