Prehabilitation for Total Knee Arthroplasty
Ellie Rubin, SPT
Background
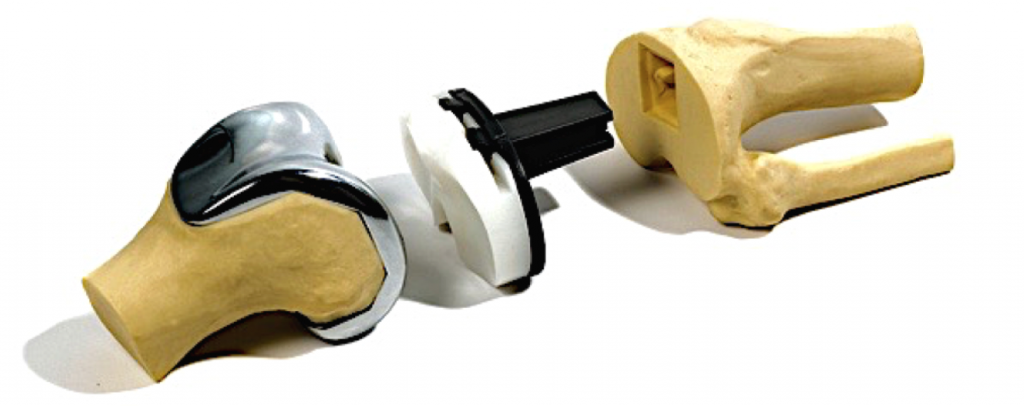
The total knee arthroplasty (TKA) procedure was first introduced to me during my acute care rotation at UNC Hospitals. In following outpatient rotations through UNC Therapy Services, I had the opportunity to provide postoperative care to patients after TKA, as well to patients who were considering TKA surgery. While patients usually recovered without issue, there were still too many that were challenged by postoperative complications, resulting in their decreased ability to perform daily activities, mobility limitations, persistent postoperative pain, participation restrictions, hospital readmission, and even revision surgery. Preoperative physical therapy or, “prehabilitation”, has shown to reduce postoperative pulmonary complications and shorten the length of hospital stay in patients undergoing elective cardiac surgery;1 however, from discussions with physical therapists, patients, and classmates, I found there to be less familiarity on the prescription of prehabilitation for TKA and its treatment effects.
Statement of Need
While postoperative physical therapy after TKA helps to optimize successful surgical outcomes and patient recovery, there is still risk for complications and adverse effects, which can result in worse outcomes for the patient, hospital, and overall healthcare system. Complications and adverse events following TKA may be caused by surgical/medical error or may occur even with delivery of high-quality care as a result of individual patient risk factors. However, it is often the case that there are many causative and correlating factors involved. While many of these issues are outside the scope of PT practice, there are several major postoperative complications associated with worse surgical outcomes that can be positively impacted by prehabilitation.
Additionally, over the last 15 years, growth in demand for TKA has risen at an exponential rate;2 this demand is expected to continue rising at increasing rate over the next 30 years. Even the most conservative of projection models project an increase in demand for primary TKA in the US to increase by at least 143% by 2050, which translates to 1.5 million TKA procedures being completed annually by 2050.3 Demand for PT services after TKA is thus increasing and innovative approaches to care delivery are required to align increasing demand with supply. Prehabilitation has been proposed as an approach to mediate demand for rehabilitation services after TKA in the short term.4
Overview and Purpose
Prehabilitation is broadly defined as improving the functional capacity of an individual through physical activity to withstand a stressful event.5 The theory of prehabilitation supports the direct and positive effects that PT before TKA can have on a patient’s preoperative physical and functional status and in reducing modifiable risk factors, thereby contributing to improved postoperative outcomes.6 While there have been multiple randomized and controlled clinical trials completed in attempt to assess the efficacy of prehabilitation before TKA, the high variability of study methods and lack of standardized prehab intervention compromises ability to make comparison between studies. Nonetheless, sample populations remain similar and assessment of methodological quality suggests low risk of bias with individual study methods. Thus, while definitive conclusions cannot be drawn from currently available research, there is still evidence, albeit limited, to suggest that prehabilitation can have clinically meaningful impact on certain post-TKA outcomes when utilizing a protocol with appropriate intervention parameters, format, and methodology.
The purpose of this capstone project is thus to educate healthcare professionals and PT students to assist with delivery of clinically-meaningful prehabilitation intervention for patients prior to TKA in order to optimize postoperative rehabilitation.
Products
During our Evidence Based Practice II course (PHYT 752), I completed a Critically Appraised Topic based on the clinical question: “For an 86-year-old male patient with knee osteoarthritis undergoing elective total knee arthroplasty, does participation in both pre- and postoperative physical therapy, compared with just postoperative physical therapy, significantly reduce the risk of postoperative complications for 90 days following surgery?”
For this capstone project, I expanded my systematic literature search to include studies comprised of patients of all ages and that measured the effect of prehabilitation on post-operative outcomes at any timepoint following TKA. Based on this literature review, I created a Prehab Evidence Table of randomized and controlled clinical trials. Based on conclusions and limitations from these RCT’s, as well as additional review of the literature to clarify the primary postoperative complications faced by TKA patients and their effect on patient outcomes, I created a Prehabilitation Protocol for clinicians to use with patients indicated for TKA. I also designed a corresponding Prehabilitation Home Exercise Program (HEP) presented in a patient-friendly handout with step-by-step written instructions and images that highlight target muscles and provide sequencing and directional cues. Finally, I created an educational Prehab PowerPoint presentation designed for healthcare professionals and students as an in-service or lecture material that synthesizes my research findings and conclusions.
Evaluation and Reflection
In order to effectively evaluate educational outcomes and allow for continued improvement of materials for future instruction, I designed 2 evaluation forms formatted on the typical five-level Likert item: one for the patient HEP handout and the other for the PowerPoint presentation.
During my final clinical rotation at an outpatient orthopedic clinic, which often treats pre- and post-op TKA patients, I plan to present my capstone products as an educational in-service. A professional development goal of mine is to improve my confidence in my ability to present material to other professionals and provide succinct and accurate clarification or elaboration on presentation content in response to follow-up questions, as I feel it will better prepare me for future provision of continuing education to practicing clinicians, as well as future clinical education instruction to DPT students. The 2 evaluation forms for the patient pre-TKA handout and PowerPoint presentation will also be administered to attendees following the in-service.
My personal learning goals for this capstone project were to: 1) Complete a long-term project composed of multiple products in accordance with a self-directed timeline; 2) Develop an extensive and effective educational module on delivery of prehabilitation intervention for patients prior to TKA; and 3) Prepare appropriate educational materials for practicing clinicians, PT students, and patients.
I have exceeded my own expectations in reaching these personal goals. I feel the products I have created work soundly together to create a clinically meaningful resource for clinicians and students who wish to deliver effective and quality prehabilitation services that improve patients’ post-TKA outcomes and can help to mediate demand for rehabilitation services after TKA in the short term.
Acknowledgements
I would like to express my gratitude to my capstone and academic advisor Dr. Mike Gross, PT, PhD, FAPTA, for his indispensable guidance in the conception of this project and helping me see it through to the end.
Thank you to Jon Hacke, PT, DPT, MA, OCS, for sharing your breadth and depth of clinical and academic expertise in orthopedic rehabilitation throughout the length of our DPT program and the additional time you graciously donated as my committee member to help me make this capstone project something I am truly proud of.
Thank you to Pete Olmos, MPT for your direction and compassion in the clinic. Your support as my clinical education instructor enabled me to build the confidence in myself that I was missing. I am so grateful for your willingness to act as my committee member and devote your time to help me improve the clinical meaningfulness of this project.
Finally, I would like to thank my family, who have supported me throughout this journey since I decided at that rest-stop off I-17 near Bumble Bee, AZ that I was going to become a PT, and my best friend and partner Eddie, for your daily love and service.
References
- Hulzebos EHJ, Smit Y, Helders PPJM, van Meeteren NLU. Preoperative physical therapy for elective cardiac surgery patients. Cochrane Database Syst Rev. 2012;(11). doi:10.1002/14651858.CD010118.pub2.
- Mehrotra C, Remington PL, Naimi TS, Washington W, Miller R. Trends in total knee replacement surgeries and implications for public health, 1990-2000. Public Health Rep. 2005;120:278–282.
- Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S. Projected increase in total knee arthroplasty in the United States – an alternative projection model. Osteoarthr Cartil. 2017;25(11):1797-1803. doi:10.1016/j.joca.2017.07.022.
- Landry MD, Jaglal SB, Wodchis WP, Cooper NS, Cott CA. Rehabilitation services after total joint replacement in Ontario, Canada: can “prehabilitation” programs mediate an increasing demand? Int J Rehabil Res Int Zeitschrift fur Rehabil Rev Int Rech Readapt. 2007;30(4):297-303. doi:10.1097/MRR.0b013e3282f14422.
- Ditmyer MM, Topp R, Pifer M. Prehabilitation in preparation for orthopaedic surgery. Orthop Nurs. 2002;21(5):43-44.
- Topp R, Swank AM, Quesada PM, Nyland J, Malkani A. The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. PM R. 2009;1(8):729-735. doi:10.1016/j.pmrj.2009.06.003.

6 Responses to “Prehabilitation for Total Knee Arthroplasty”
Elinor Rubin
Hi Kate,
In one of the RCTs that I appraised by Beaupre et al (1), the prehab intervention consisted of pre-operative education on completion of ADLs and functional tasks post-operatively, in addition to the therapeutic exercise intervention. Subjects that received this prehab intervention had an average length of hospital stay following surgery that was, on average, 1 day less than the control subjects. Additionally, there was a difference between the experimental and control groups in terms of discharge location: 35% of subjects that received prehab were transferred to subacute rehab following surgery, compared with the 47% from the control group. While the authors did not specifically credit the pre-op education as the reason for these outcomes, it does seem to me that it certainly may have come into play.
I agree that patients with knee OA would benefit from PT earlier on in the disease process. In another RCT by Calatayud et al(2), two of the subjects that received prehab intervention actually cancelled their scheduled TKA surgery due to their level of functional gains. This study, in particular, had subjects attend a greater number of prehab sessions, which they attribute to the success of the intervention. With earlier intervention, I think a big focus of treatment also needs to be on behavior change, especially weight loss management. Less force across the damaged joint would help to slow further degradation and reduce pain, and thus improve ability to complete daily activities as well as overall physical function. Obesity is a risk factor for almost every post-operative complication, not just because of the physiological effects of obesity, but also because of the functional limitations it places on people. If we can help get patients out of this negative progression earlier on in the disease process, I certainly think there would be benefits across the health spectrum and disease timeline.
1. Beaupre L, Lier D, Davies D, Johnston D. The effect of a preoperative exercise and education program on functional recovery, health related quality of life, and health service utilization following primary total knee arthroplasty. J Rheumatol. 2004;31(6):1166-1173.
2. Calatayud J, Casana J, Ezzatvar Y, Jakobsen MD, Sundstrup E, Andersen LL. High-intensity preoperative training improves physical and functional recovery in the early post-operative periods after total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2864-2872. doi:10.1007/s00167-016-3985-5.
takumik
Hi Ellie,
I really appreciate all the products and works done in your capstone as they are very extensive and ready to use for education to both patients and clinicians. Particularly, I’m impressed by your phenomenal work on literature review based on the number of referred articles in protocol and powerpoint!! With that being said, I think you made a great running start or “pre”start of your professional career of clinicians and educator.
In terms of the topic, I also really believe that prerehab for TKA would be better outcome than just post-op rehab for the most patients. But, unfortunately, availability of prerehab really depends on facility and physician’s referral as I have experienced several setting including where I have done prerehab for TKA. It was nice that you talked about “mediate patient expectation” as such problem is commonly seem in clinic. By doing prerehab, you never know if patients experience pain relief just by conservative management. For those who has never done PT before surgery, people tend to believe that “TKA fixes everything” which is not necessarily true. The opportunity of providing education about expectation of post-op management including PT would reduce such misbelief and avoid the vicious cycle of chronic pain as you talked.
Great Job, Ellie
Tak-
Carla Hill
Ellie,
Great job on your Capstone with an extensive review of the literature related to post-TKA complications and benefits of prehabilitation. Often patients get an educational session about what to expect during their hospital stay but could certainly benefit from more PT ahead of time to help them physically prepare for the post-op phase. It will be interesting to see if this becomes more standard as healthcare moves toward value-based care.
Carla
Kate Finegan
Hi Ellie!
I thought that your capstone was absolutely fantastic! As we started this process earlier on in the year, prehabilitation for joint replacements crossed my mind and I wondered if anyone might choose a topic along those lines. So when I saw your page, I was very excited. First and foremost, your prehabilitation protocol was extremely detailed and comprehensive, but easy to follow. I appreciate the specificity with which you discussed the intervention activities and their parameters. I spent a few days of my acute care rotation in the joint unit, where I was incredibly impressed with the fact that they were seeing patients post-op day 0 and 1. It is truly incredible to think that we still have room to improve this area of practice. I will say that I also saw some pediatric patients who underwent various hip surgeries under this particular surgeon who requires prehabilitation, and they were so incredibly impressive and quick to progress. He only required one visit to educate the patients on their precautions, how to transfer from the bed while adhering to precautions, and gait using crutches. Did you happen to find anything in your research about how education on these functional topics impact outcomes for patients post-TKA? My other question in regards to your project was if you thought that this protocol could be implemented even earlier on in the disease process of OA, say even before the patient decides to undergo surgery? I ask because I feel as if this program is a great thing to get patients started on as early as possible in order to make it routine and also potentially slow the timeline for joint replacement. Great job Ellie!
Jaime Hankins
Hi Ellie,
This information is fantastic! Having had this same rotation, I also know the issues many patients face post-op. My own mom had two knee replacements and each time I tried to do some of my own research to give some exercises to help her gain a little bit of advantage going into surgery as she had many years of pain that physically limited her. I wish I would have had this information to not only show her exercises she could do but to also give her information about improved post-op outcomes. As you pointed out, there are a huge number of people electing to have this surgery so your products can be very important for them and possibly easy to implement at pre-surgery information sessions. Great job!
Jeremy Bradford
Elinor,
You have put together a fine capstone, and I can tell that you put a lot of work into this. I readily acknowledge the necessity for your capstone given the likelihood of more and more TKAs in the future. I’ve worked with TKA in the past and expect see it many more times. Yes, productive prehabilitation will improve outcomes. That much I already suspected, but honestly I would not have known how to go about putting together a solid plan without doing some research. You’ve done the research for me! Your TKA protocols are thorough, and I really like that you so clearly outlined the clinical reasoning for the protocols. That additional information gives me confidence in the protocols and also enhances my clinical judgment since I can compare my patient findings with the reasoning that you’ve listed. Having the parameters for the exercises laid out is also very convenient, especially for a new clinician (or and old hand not familiar with this sort of case). The Appendix B has a high level of utility given that it is succinct, visual, and precise. Hats off to a job well done!