Bridging the Gap: Transition from Hospital to Home for SCI
Sara Galante, SPT & Austin White, SPT
Background
Our passion for patient education and working with individuals who have neurological injuries brought us together as teammates for our second year “Managing Contemporary Practice” course project. Although our idea for the project did not fit that class’ learning objectives, we were passionate about pursuing the idea later. During our second year rotations, we gained the background needed in order to pursue filling a need in the current system. We knew this was a big idea that would take a lot of work, and luckily, the Capstone curriculum was the perfect opportunity to create the first draft of our passion project that we hope to expand throughout our future careers. We worked together as a team on every aspect of this project, we shared the same adviser and committee, and now we share a Capstone website for you to see the culmination of our hard work.
Sara’s Background
My passion for rehab began volunteering on UNC’s 7th floor inpatient unit, organizing the assistive devices closet and helping with wheelchair follows. I further got to explore that passion on my second rotation at inpatient rehab in Charlotte, working on the Spinal Cord Injury (SCI) team and conducting patient education classes on topics related to transition to home. I knew that logistically this was the perfect opportunity for education, yet some patients were worn out, confused by the language, or weren’t psychologically ready to hear this information. Now they were missing out on information they needed to know, information that could keep them out of the hospital later. This was anecdotally confirmed for me on my third rotation, when I saw one of my previous patients from rehab admitted to acute care with secondary complications from his injury. I called Austin on my way home this day and told her about how our idea had come full circle.
Austin’s Background
My heart has always been with inpatient rehab and patients with neurological injuries. I find it really fulfilling to work on functional mobility and provide education to patients and their caregivers to facilitate the transition back home after a (typically) traumatic experience. While witnessing a family friend navigate his return home after an SCI, I noticed the “telephone effect” that occurred as he and his primary caregiver (his wife) had to teach new hired caregivers how to perform dependent transfers based on what they remembered from the overwhelming time in inpatient rehab. Despite the wonderful care and education while in rehab, there was still a gap in terms of caregiver resources to help ease the burden on the family to train other caregivers. During my third rotation at an inpatient rehab facility in Wilmington, I too noticed the impact of learning readiness on patient education. Therefore, when Sara called on her way home from work one day, we decided Capstone was an opportunity to pursue our patient education idea.
Statement of Need
While our ultimate hopes and dreams are that this could one day turn into an all-inclusive website for all levels of SCI covering many different topics, we have narrowed our focus for this project. The functional level of the target audience will include those that have periscapular and shoulder mobility, lack hand function/fine motor control, and require assistance from caregivers for ADLs and transfers. This subgroup is important to address within the SCI population, as their limited independent mobility requires the development of direction of care skills to communicate with caregivers to optimize their autonomy.
Conversations with healthcare providers, caregivers, individuals with SCI, and our literature review revealed that more focus should be devoted to the transition period from hospital to home. Barriers arise after the transition to home, as evidenced by the development of secondary conditions, hospital readmissions, and health complications in the SCI population.1-4 This Capstone idea to create easily accessible, online videos will help bridge some of the education gaps during the caregiver shift from the PTs and nurses in rehab to the families and spouses at home.5
A current online resource for the SCI population called “Voices of Experience” does include some online educational videos; however, it does not include direction of care, which is why the need for our particular product still exists.
Overview & Purpose
Our Capstone project is intended to meet the above need through evidence-based strategies, including the intentional timing, use of peer mentors, online video format, and topic of direction of care.
The available literature indicates adult learners need to be ready for learning in order to successfully implement new information;6 however, with the coping that is initially required after SCI, many are unable to learn when they have access to education at the hospital before the transition to home.7-9
Education via peer mentoring is well supported in the literature,1,2,10 yet the outpatient healthcare providers all described how difficult it is to access peer mentors in the community as compared to while in the hospital. In contrast to other supportive relationships, the benefits of peer mentors include credibility and normalization as well as increased quality of life and self-efficacy.2,10
The online video format is an effective education delivery method, as evidenced by the nearly six-time greater reach of the online format in just one third of the amount of time with a wide geographic distribution of the audience.5 Furthermore, given the functional level of our target audience, online videos decrease the amount of assistance required from caregivers as compared to in-person education sessions.
Successful direction of care incorporates self-awareness of the body, clear and specific communication, confidence to self-advocate, problem-solving skills, patience, and flexibility.4 The current development of an outcome measure to directly assess the ability of individuals with SCI to direct care and caregiving suggests that this is a topic of growing interest and importance in the SCI population.4
Health Literacy
Many standard-of-care education formats (i.e. generic handouts provided during rehab) are delivered via methods that are not health-literacy friendly, and the recipients fail to understand and find relevance in the material.2 The use of peer educators helps achieve health literacy in our videos by limiting the amount of medical terminology used and lowering the reading level of material. In addition, a video format removes the reading comprehension component, making the material more accessible. From our literature review, we know there is a lack of research examining health-literacy conscious patient education for individuals with SCI. However, utilizing the peer mentors under the direction of a PT is not harmful and qualitative data suggests that patients preferred peers.2,3,7-9,11
Products
Our evidence table and literature review provides evidence-based support for the strategies used in the two Capstone products.
We created two peer mentor videos on the topic of direction of care. Two different peer mentors were featured to relate to different members of the target audience.
Giovanna is a young adult who has a C6 incomplete SCI (ASIA B) who discusses her transition from hospital to home including how her relationships changed and what she wishes she knew during that time.
Paul is an older adult who has a C4 incomplete SCI (ASIA C) who discusses his transition from hospital to home including his experience hiring paid caregivers and current challenges while directing care. Paul also models how he directs care while eating dinner and changing his contacts.
Our ultimate goal is that these videos will eventually be housed on a website for all levels of SCI covering many different topics for individuals with SCI and their caregivers.
Evaluation
Due to extenuating circumstances, we were not able to visit the North Carolina Spinal Cord Injury Association (NCSCIA) support groups as originally planned to present and evaluate our videos in person. Therefore, to assess our videos, we reached out to individuals with SCI in the community and clinicians who frequently work with this population to watch the videos online and submit feedback on a Qualtrics survey. This led to a small sample size of 11 responses, including four responses from individuals with SCI. Some statements were not applicable to all viewers, and thus 11 responses were not recorded for every statement.
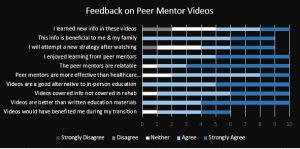
Consistent with the literature, all viewers enjoyed learning from a peer mentor with 54.55% strongly agreeing. The peer mentor was relatable for 90% of viewers including 20% who agreed and 70% who strongly agreed. All viewers agreed (36.36%) or strongly agreed (63.64%) that the video format was a better way to present this information than written formats currently used for most patient education. Again consistent with the literature, all of the viewers with SCI (n=4) agreed (50%) or strongly agreed (50%) that the peer mentor was more effective than other healthcare providers or experts at conveying this information.
Interesting comments included: “I would’ve enjoyed seeing it in rehab! Though, it might have scared me a little bit…” and “I think the patient should decide for themselves when to watch it and whether or not they want to.” These statements reflect our earlier instincts that the timing of this beneficial education will be different for everyone, meaning online access to the material fills this need. The evaluation step has led to feedback that indicates what videos are needed as we expand this project in the future.
Reflections
Sara’s Reflection
This has been one of the most challenging and rewarding experiences of PT school thus far. Growing up as a “creative type,” I always thought I would be pursuing an artistic avenue after college and while my path brought me to PT, I now realize I can do both. Learning a new skill (video and editing) for this project was daunting, but something I have been wanting to do for a while. The process of developing our final products challenged me to be creative yet realistic, something difficult as my ambition often exceeds my available hours in a day. An idea like this is necessary, and the world is changing so quickly that technology is one of the only avenues for communication and building relationships. Even though COVID-19 forced us to adapt and change direction on a few components of our project, I realize the potential of this idea now more than ever. Patients are still in the hospital, they would still benefit from learning from a peer, yet don’t have access to one.
This was also one of the first times that I searched for research and found almost nothing. The process of searching and writing the literature review over the past 2 semesters really made me grow my clinical reasoning skills and help solve a problem the literature hasn’t addressed yet. Maybe, in time, we will help answer these questions with research of our own. Another unintended benefit of the lack of literature was the professional connections we gained as we sought out expert opinions during this experience. I had a great excuse to converse with and pick the brains of some amazing mentors in this field from program developers, to other allied health professors, to previous CIs, and a PT I used to shadow as an undergraduate.
Finally, it is incredibly fulfilling for me to have the first step of a passion project with one of my best friends and amazing future colleagues. It’s been a hard three years of laughing, crying and every emotion in between and I don’t think I could have gone through this creative process with anyone but her. After several project pivots, new ideas, and brainstorming sessions, it’s amazing she still want to work with me on this but I am excited about being in it for the long-haul!
Austin’s Reflection
It has been an incredibly rewarding experience to discover a need and fill that gap with a tangible resource that can be used in the future. While I’m so proud of these two peer mentor videos for our Capstone project, I’m equally as excited about continuing this project with one of my dearest friends throughout our careers incorporating the feedback we received. It is really fulfilling to know this is the beginning of something that could be really special rather than just the end of an assignment.
Collaboration with several different key stakeholders has also been a highlight of the experience for me. I loved being able to connect and have conversations with interdisciplinary professionals (including PTs, OTs, and the chairman of the NCSCIA) from a wide range of settings and individuals with SCI at different stages of recovery in a variety of locations around the state (thank you social media!). These professionals have become valuable mentors and for that I am so grateful. This collaboration helped build my communication skills, but it also gave me so much perspective and respect for each and every voice as they all contributed valuable insight. The collaboration with key stakeholders also highlighted the fact that there is a clear need here, yet how to fill that need is difficult due to the individuality that accompanies learning readiness after a traumatic SCI and the emphasis on productivity for clinicians that limits time available for passion projects such as this one.
This experience has also been a learning lesson on the importance of flexibility, as this project took many pivots as we navigated stakeholder conversations and learned what was realistically possible. For example, while we originally planned to show an example of a dependent transfer, we also recognized the boundaries of respecting what our volunteers were comfortable with doing and sharing as it meant so much that they were willing to be so open about this vulnerable time in their lives. Another example was the impact of COVID-19, which limited our ability to incorporate committee and evaluation feedback into the final products. We could not re-film any interview segments based on feedback in an attempt to keep our peer mentors safe and healthy, but it further reiterated that this is the beginning (not the end) of this passion project.
Acknowledgements
First and foremost, we would like to give a huge thank you to Giovanna, Paul, and their families for opening up their homes and hearts to us. While in these videos they serve as peer mentors for individuals with SCI, their desire to help others by being open and vulnerable about a challenging time in their lives is something that we can all learn from.
To Dr. Vicki Mercer, PT, DPT, thank you for your patience with our pivots and for grounding us when narrowing the focus of our larger-than-life aspirations was necessary.
To Raheleh Tschoepe, MS, OTR/L, thank you for providing calm and tangible guidance during our creative struggles and introducing us to our peer mentors for these videos.
To Dr. Austin Leedy, PT, DPT, thank you for fostering love for this underserved patient population, bouncing ideas back and forth at coffee shops, and providing a unique perspective from the acute care setting when a patient’s journey begins.
To Dr. Audrey Osinski, PT, DPT, NCS, MSCS, thank you for connecting us with experts in the triangle, providing expertise yourself, and being involved from start to finish from initial brainstorming to problem-solving through the difficulties due to COVID-19.
To Debbie Meyers from the NCSCIA, thank you for your expertise that helped us narrow our focus early on and for inviting us to attend the local SCI support groups.
Finally, thank you to all of our classmates in the Class of 2020! Your support and love allowed us to grow and fearlessly pursue our passion despite the hard work it would take. Thank you for an amazing 3 years and we can’t wait to see the amazing group of clinicians you’ll be!
References
- Jones ML, Gassaway J, Sweatman WM. Peer mentoring reduces unplanned readmissions and improves self-efficacy following inpatient rehabilitation for individuals with spinal cord injury. J Spinal Cord Med.2019:1-9. doi:10.1080/10790268.2019.1645407.
- Chaffey L, Bigby C. Health Education by Peers with Spinal Cord Injury: a Scoping Review. J Dev Phys Disabil.2017;30(1):1-14. doi:10.1007/s10882-017-9569-6.
- Schubart J. An e-learning program to prevent pressure ulcers in adults with spinal cord injury: a pre- and post- pilot test among rehabilitation patients following discharge to home. Ostomy. Wound. Manage.2012;58(10):38-49.
- Zanca JM. Systematic Assessment of Caregiving Skill Performance by Individuals with Tetraplegia and Their Caregivers. Kessler Foundation.2017.
- Hoffman J, Salzman C, Garbaccio C, Burns SP, Crane D, Bombardier C. Use of on-demand video to provide patient education on spinal cord injury. J Spinal Cord Med.2011;34(4):404-409. doi:10.1179/2045772311Y.0000000015.
- Whiteneck GG, Gassaway J, Dijkers MP, et al. Inpatient and postdischarge rehabilitation services provided in the first year after spinal cord injury: findings from the SCIRehab Study. Arch. Phys. Med. Rehabil.2011;92(3):361-368. doi:10.1016/j.apmr.2010.07.241.
- Bernet M, Sommerhalder K, Mischke C, Hahn S, Wyss A. “theory does not get you from bed to wheelchair”: A qualitative study on patients’ views of an education program in spinal cord injury rehabilitation. Rehabil. Nurs.2019;44(5):247-253. doi:10.1097/rnj.0000000000000175.
- van Wyk K, Backwell A, Townson A. A narrative literature review to direct spinal cord injury patient education programming. Top. Spinal Cord Inj. Rehabil.2015;21(1):49-60. doi:10.1310/sci2101-49.
- May L, Day R, Warren S. Evaluation of patient education in spinal cord injury rehabilitation: knowledge, problem-solving and perceived importance. Disabil. Rehabil.2006;28(7):405-413. doi:10.1080/09638280500192439.
- Skeels SE, Pernigotti D, Houlihan BV, et al. SCI peer health coach influence on self-management with peers: a qualitative analysis. Spinal Cord.2017;55(11):1016-1022. doi:10.1038/sc.2017.104.
- Gassaway J, Jones ML, Sweatman WM, Young T. Peer-led, transformative learning approaches increase classroom engagement in care self-management classes during inpatient rehabilitation of individuals with spinal cord injury. J Spinal Cord Med.2019;42(3):338-346. doi:10.1080/10790268.2017.1385992.


13 Responses to “Bridging the Gap: Transition from Hospital to Home for SCI”
karlak
Austin and Sara,
WOW! You guys are so awesome and I am so proud of y’all for the hard work you put into this. I remember you talking about this/ brainstorming ideas last year, and it is great to see the product of all your hard work!
These videos are GREAT, and I love that you stated these are just the start of what could be a massive resource center for these patients, caregivers, students, and more. I agree that using videos is a fantastic way to access more individuals, and eliminates some factors such as literacy level. I also think that this allows you to reach a greater population of people. Now anyone ( with access to internet and a computer/phone) can find these resources in one place and easily come back to them for reference. I think this is a much better way to provide for patients versus handouts given at a clinic.
Also, I especially enjoy that these are coming directly from the patient. The patients are definitely the ones that know best about their care ( at least most of the time). So instead of referring these questions off to caregivers, or their medical team, you went directly to THEM. I feel like this does not happen enough in the medical community, and instead often the patient can be forgotten. So instead of only using other professionals or caregivers, let’s give the patients the opportunity to share what is important to them and how they need to be cared for!
Once again, awesome job! Not only on your products, but also designing something that seems so pertinent to the healthcare of our patients!
Austin White
Hello!
Hannah, thank you so much for watching our videos and reading our literature review! It is really encouraging to hear excitement from our classmates because it suggests that now y’all are aware of this gap as well, which at the end of the day awareness is a benefit of completing this project. I’m so glad you found Appendix A from the Zanca article helpful! Personally, I’m a huge fan of Zanca’s work as I love that they are working to create an assessment that will be able to measure direction of care (i.e. assistance management in the Teaching Effective Assistance Management “TEAM” tool). Having an outcome measure will support the opportunity for more research in this area, which is necessary and will be helpful to the SCI population.
Audrey, I smiled so much reading your comment because your support means the world to Sara and me! We feel lucky to have had you on our committee, especially given all that you have going on in your own career. I truly hope my path crosses with yours again in the future!
Thanks again for all of the support and kind words & stay safe!
Austin
Audrey Osinski
Congratulations on completing your great capstone project, Austin and Sara! You two did a wonderful job and as you mentioned, have set a foundation for very helpful educational materials in the future! It would be great to have a library of peer mentor videos with various topics to help our patients with SCI! It was a pleasure to be on your committee – please keep in touch.
Best,
Audrey
Hannah Ryan
Sara and Austin,
I remember hearing you two talk about this project, and I was so excited to see the results of the implementation of your wonderful idea. I hope that others will use your idea to create informative videos that allow for peer mentorship for other patient populations as well. As Emma mentioned, this is also an important time to have more virtual information for patients.
Your videos truly help meet the important factors for positive outcomes discussed in your summary such as improving ability to self-advocate. I think Appendix A is very helpful. As a therapist, it is important to understand the challenges and possible solutions (“key suggestions”) to the patient-caregiver relationship because we can offer resources and suggestions to help overcome these challenges. I really appreciate your hard work and dedication in completing this important project. I hope to use the videos and the information I learned from your evidence summary in my future practice. Great work!
Best,
Hannah
Sara Galante
Vickie & Debby- Thank you for your endless support through this project! Makes me extremely happy that you both were able to see the amount of work we put into this project.
Amelia & Jake- Thank you for your kind words! Austin hit most of the points I was going to touch on, but your feedback and ideas are definitely things to take into consideration moving forward. Ultimately, we wanted to be able to include so many of your points in this project but there just wasn’t time to match our aspirations.
Emma- You make a great point about inclusion with this project and I applaud your continued advocacy for underserved populations in every project during PT school and beyond. Unfortunately, both the mentors and the individuals who gave feedback on this project were out of convenience due the nature of the beast we were undertaking. We tossed around many ideas during the timeline of development, including translating the videos into Spanish for Guatemala, but ultimately did not have the time nor resources. Ultimately I would love to include different injury levels, ethnicities, and languages in our dream resource to increase accessibility and relate-ability for all patients. Over my last two rotations, a majority of my patients were of ethnicities not included in this project and I would love to change that in the future. Just as we learned about these individual’s barriers to transitioning home in an interview, I would love to be able to learn more about cultural-specific barriers by interviewing other individuals. Additionally, for people who are uninsured or undocumented, relying on government resources that are unfamiliar or in a different language is scary, especially when interpreters were not always available and many of the resources are only in English (classes, books, pamphlets). Additionally, underrepresentation of minority populations within peer mentors and the professions of PT, OT, and Speech make it difficult for patients to be able to relate and trust their therapists. Obviously these are also systemic problems, but instances I have seen nonetheless. Maybe in the future we can recruit your help for locating possible mentors and/or as a PT/ interpreter to get the representation we would ideally like to have!
Joe- We would be honored if you used our videos in the future! We hope this can be a resource for the clinics who don’t have access to peer mentors, can’t access one at this time, or for the patients who would benefit from one but are not yet ready to have these conversations. The peer mentor model was something we knew we needed but was one of the most difficult parts (feasibility-wise) because it meant that we were relying on other people to complete our project. That is why we are so grateful to Paul, Giovanna, and their families and really admire their desire to give back and help someone else! It’s funny that you mention that our products could contribute to research because Austin and I often commented that we were “skipping a step” in this project by seeing a need and jumping straight into filling it without the research to back us up. From our discussions with key stakeholders, we learned that the lack of research is one of the reasons this resource doesn’t yet exist, although it would be difficult to conduct this research without a resource. Hopefully we can change that! Thank you so much for you kind and encouraging words!
Sara
Joe Douglass
Austin and Sara,
What an amazing Capstone project! The steps you all have taken this year has no doubt set a foundation for turning this school project into a real online resource for individuals with SCI and their caregivers. I really appreciate the practicality and feasibility of your project.
There clearly is a need for a product like this. Incorporating the peer-mentor model was an excellent idea, as this has proven effective for other populations (Wang et al). Maybe your products can contribute to the paucity of research in this area, and hopefully prove efficacious.
A resource like the one you all plan to create will prove vital to education for patients, caregivers, and clinicians around the world. I, for one, will be looking to use these videos whenever I have a patient who has recently experienced an SCI and is in a period of transition.
Great work!
Best,
Joe
Wang EA, Hong CS, Samuels L, Shavit S, Sanders R, Kushel M. Transitions clinic: creating a community-based model of health care for recently released California prisoners. Public Health Rep. 2010;125(2):171-177. doi:10.1177/003335491012500205
Austin White
Amelia & Jake,
Thank you so much for your support of our Capstone videos and encouragement to keep going with the project! It means a lot that you also see this area as a clear need. The more clinicians are able to see it as a need, the more both inpatient (upon discharge) and outpatient (during their POC) PTs can recommend resources, such as the videos we have created and hope to create more of! Since you both brought up similar points about the caregiver experience, I’m going to reply to both of you here.
Amelia, great question about similar resources for caregivers! This was actually the subject of my CAT during EBP II this past fall, and I learned a lot about caregiver education. The limited published research and abundance of studies in the recruitment phase (as evidenced by searching ClinicalTrials.gov) illustrates that caregiver education for the SCI population is of growing interest and importance. I would be more than happy to share my CAT with you, but the main takeaways are that 1) there are several studies confirming the negative caregiver outcomes (biopsychosocial in nature) that suggest caregiver education as a solution and 2) there is emerging, promising support for problem-solving training for this caregiver population.
Jake, I agree with you that the insight both Giovanna and Paul provided on the dynamic of relationships is powerful! During my research on the caregiver experience this past fall, I came across an article by Jeyathevan et al. (full citation below) that discusses re-building relationships after an SCI in which the dynamic of spouse caregiver-care recipient relationships and parent-child caregiver-care recipient relationships are addressed. This is an article that I shared with our peer mentors to reassure them that they are not alone in this experience and to provide (hopefully) helpful coping strategies to maintain their relationships.
For these reasons and others that y’all brought up, we do plan to include caregiver perspective videos and resources on our eventual website that houses many videos for the SCI population. However, we had to scale back for the purposes of this Capstone project, and we felt both Giovanna and Paul were too amazing to pass up spreading their wisdom and experiences to others! We are so appreciative that both of them spoke so vulnerably about the relationship dynamic to open this conversation for the future and to allow other individuals with SCI who watch the videos to realize they are not alone in that challenge either.
Again, thank you both so much for your thoughtful responses! Your willingness to dive deeper into this topic means so much to me.
Jeyathevan G, Cameron JI, Craven BC, Munce SEP, Jaglal SB. Re-building relationships after a spinal cord injury: experiences of family caregivers and care recipients. BMC Neurol. 2019;19(1):117. doi:10.1186/s12883-019-1347-x.
Jake Tyson
Austin & Sara,
WOW, what a job well done!! This project is extremely comprehensive, fills a much-needed gap, and is very patient-centered and accessible for all levels of health literacy. I will certainly be using these resources in the future, as I will have my last rotation in in-patient rehabilitation this summer. This is super helpful for getting me thinking about what patients needs may be so I can anticipate them, as Giovanna describes that anticipation of needs is incredibly important. I will certainly be using your resources as “cheat sheets” throughout my rotation and during my career working with individuals with neurological injuries and conditions!
I really respect your dedication to this project even despite the many barriers that arose due to COVID-19. Unfortunately, strokes, SCIs, TBIs, etc do not cease during a global pandemic. It is likely even harder for these people to get the care they need during this time, which further increases the need for peer mentoring. By providing peer mentoring videos online, you will be able to reach more people virtually without them having to be physically present. This is a reminder of how much of patient/caregiver education can be done over virtual formats such as YouTube and Zoom, which is a valuable and necessary feature of PT care during this time. I suspect there is a huge opportunity for Telehealth PT sessions with involvement of caregivers throughout in-patient rehab and post-discharge! This project provides direction on how to navigate this territory virtually and effectively.
I especially appreciate the interviews you did with Giovanna and Paul. These contain very valuable information that will be highly relatable for many patients as they navigate the difficult transition from the hospital to home. I am glad that you tackled psychosocial issues that may greatly impact quality of life, but that many professionals may not see to be in their scope. Giovanna and Paul’s descriptions of the changing dynamics of their romantic relationships following injury were authentic and thought-provoking. Transitioning from being someone’s partner to being their partner AND caretaker must be extremely difficult and even traumatic in some ways. This really emphasizes the need for caretaker education and counseling that teaches couples to thrive in this new environment without sacrificing intimacy. Your advice of self-advocating with clear and specific communication, and “keeping it light-hearted” is very helpful for this purpose.
Above all, I am extremely inspired and impressed by the dedication, passion, and value you have put into this project. I am so excited to see how this project will evolve over time as you two enter your final rotation and your promising careers after graduating. Keep up the EXCELLENT work!!!
-Jake
Amelia Cain
Austin and Sara,
Really excellent idea and execution, I’m impressed! You are absolutely filling a gap in care with this project. I appreciate that you have thoroughly considered what the need is and how to address it. For example, you have recognized the importance of timing of information, the value of peer mentoring, and the accessibility of online video resources. This project provides a valuable resource and I hope that it does continue to grow with more videos and expanded representation. Really exceptional job.
I do have a couple of potential considerations as the project expands (which are certainly out of the scope of this current project). I see that this was an interdisciplinary effort including OTs and the chairman of the NCSCIA, have you considering reaching out to rehabilitation counselors or psychologists or other providers who may focus on interpersonal relationships or directing care after an injury? In your research, have you come across any similar resources for caregivers or carepartners, since this can be a bit of a two-way street? Finally, what are your thoughts on when and how this resource would be accessed? For example, is the hope that physical therapists or other providers could recommend it to patients they are working with, that it would be available via google search to anyone seeking it out, or maybe that it would be included as a recommended resource as people are leaving the hospital? As you all stated, adult learners need to be ready to learn but may not be able to before transitioning to home–so how do we make sure those who might benefit from this resource are able to access it in a timely manner?
Again, thank you both for your hard work and dedication to such an excellent project, as well as your perseverance and adaptability in such volatile times. I’m grateful to know you both.
Austin White
Vicki and Debbie,
Thank you so much for the kind, supportive words regarding how our Capstone project turned out! We too are really happy with the results, and it has motivated us even more (as you noticed Debbie) to stay committed to this passion project in the future. Thank you both for the brainstorming sessions to guide this project during the early stages, we are so thankful y’all gave us the opportunity to see our idea come to fruition. Thanks again and hope y’all are staying safe and healthy during this time.
Debbie Thorpe
Sara and Austin
You really “hit it out of the park” with this project. I could feel both of your enthusiasm as read your reflections! The videos are amazing and will be such a welcome resource for patients and clinicians. You both should be very proud of your products and the way you worked as a “team”!
Best Wishes…
Emma Shirley
Austin & Sara,
This is a really wonderful video series of high quality content that is patient-centered and evidence-based, as well as friendly for varied levels of health literacy. I particularly honor your abilities to complete this unique and multi-faceted project in the face of numerous obstacles, including a global pandemic and international travel border closures! Your passions and care for this population really shine through the high quality of this work.
I would to hear your opinions regarding representation. According to the National Spinal Cord Injury Statistics Center, approximately 40% of new SCIs occurred with minority populations. More specifically, approximately 23% of new SCIs in 2015 to the time of the data sheet publication in 2019 were acquired by non-Hispanic, black patients and 13.2% by Hispanic patients (https://www.nscisc.uab.edu/Public/Facts%20and%20Figures%202019%20-%20Final.pdf). Moving forward with the bigger picture towards a broad website with an assortment of videos and resources, will you consider seeking out individuals with SCI from minority populations to increase representation? Referencing the transition from hospital to home, do you think that individuals with SCI that belong to minority groups have differing needs from individuals of majority groups with SCI; and if so, how might meet these needs in this video series? Furthermore, in regards to Hispanic minority populations, a personal passion of mine, did you encounter any anecdotes regarding language barriers and SCI rehabilitation and how that may affect the transition from hospital to home?
A lot of questions, I know! This is a wonderful project that fills a large need in this patient population. There are so many directions in which to grow it. I am very excited to see how the two of you transform the project in the future.
Vicki Mercer
Sara & Austin – Excellent work! I’m very pleased with this capstone project and excited to see where you will go with this in the future! Best wishes –