Background
During my time in the Doctor of Physical Therapy program I had the opportunity to gain pediatric experience through our didactic education. During our first year Motor Development course I became fascinated with infant development and musculoskeletal conditions of infants. I had another opportunity to study infant conditions and NICU physical therapy practice in PHYT 880 Child and Family Assessment in my third year. I became fascinated by NICU therapy and the lack of literature surrounding neonatal interventions. During the fall of my third year, I completed a research elective with Dr. Dana McCarty. I completed a literature review on current evidence on the effects of mechanical ventilation on cranial molding in preterm infants and on the effect of positioning on oxygenation and ventilation parameters. I realized that there was a large literature gap concerning different types of mechanical ventilation and effects on cranial molding. This is particularly pertinent as UNC changed the model of CPAP machine used in their NICU last year. This project has given me the opportunity to help synthesize and present the data collected by Dr. McCarty to help bridge this gap. The goal of this project was to determine cranial molding changes over time in preterm infants using the different CPAP systems and determine any change in frequency of infant positions (supine, sidelying, prone) between cohorts.
Statement of Need
Cranial deformities are a relatively common diagnosis in preterm infants. Deformities can be divided into abnormal proportion of cranial length and width (symmetrical) and disturbed cranial symmetry (asymmetrical).1 Plagiocephaly and brachycephaly are commonly described deformities in term newborns while dolichocephaly is reported as a specific head deformity in preterm infants.1 Despite the high prevalence of cranial deformities there is a lack of education among providers and laypersons about cranial deformity diagnosis and treatment. When presented with videos of infant craniums and objective measurements, pediatricians and other medical doctors had a significantly lower chance of correctly identifying cranial deformities than neonatal specialists.2 The perceived rating of asymmetry was more accurately assessed by parents than by clinicians without experience with cranial deformation.2 Mild-to-moderate cranial deformities (CVAI 7-12%) are much less likely to be noticed by parents or clinicians and therefore less likely to be diagnosed and treated.3 Many clinicians consider cranial deformities to be minor deficits and purely cosmetic, despite the risk for long-term musculoskeletal and cognitive deficits.4 The combination of impaired ability to accurately perceive cranial asymmetries and provider beliefs on the severity of the deformation can lead to poor care for patients with cranial deformities.
This project serves to educate fellow clinicians on identifying cranial deformities and risk factors for development. The project will include definitions of different deformities, objective measurements used to diagnose deformities, and risk factors for development of cranial deformities. The project also serves to bridge a gap in the literature surrounding the impact of different types of CPAP machines on head growth and development of dolichocephaly.
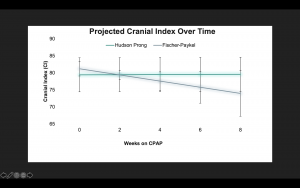
Prolonged mechanical ventilation and CPAP use has been identified as a risk factor for developing cranial abnormalities in preterm infants,5–7 but there is no current evidence assessing whether certain types of CPAP machines are more likely to cause musculoskeletal abnormalities than others. The purpose of this project is to provide education on the definition and diagnosis of cranial deformities in preterm infants while discussing the data from research on the effects of different CPAP machines on head growth and development of abnormal cranial molding.
Learning Objectives
- Identify characteristics unique to neonatal bone and cranium that make it susceptible to deformations.
- Identify and differentiate different infant cranial deformations.
- Describe the different quantitative measurements of cranial development and what they indicate.
- Explain the role of extended CPAP use and positioning on cranial development in preterm infants.
- Explain the role of extended CPAP use and positioning on oxygenation in preterm infants.
- Summarize the results of the research study.
- Synthesize and summarize implications for future research projects and practice.
Product Links
VoiceThread Presentation: https://unc.voicethread.com/share/17191266/
Literature Table: Literature Table
Literature Summary: Literature Summary Final
Critically Appraised Topic: CRITICALLY APPRAISED TOPIC
Evaluation
Feedback was given and incorporated throughout my research credit and capstone project by my advisor, Dr. Dana McCarty. This included feedback on the creation of a literature summary, evidence table, and assessment of data. Dr. McCarty gave input on the creation of the final product and the other requirements of the capstone project. This project and it’s products were made in conjunction with Ashely Hite. Ashely and I also collaborated during this time to create a poster with audio and submit to the Graduate Interprofessional Education research fair (IPE). A final evaluation form was created in order to receive feedback regarding quality of products, usefulness to clinicians, and future research opportunities.
https://docs.google.com/forms/d/1gib2m6ieADQ1V8n46bfZHWBZlf-HT9p0McmftpHv2L4/edit
Self-Reflection
I am proud of the work I put into this project. Neonatal physical therapy is a very narrow field and it is a long term goal of mine to be a NICU therapist. This project taught me how to sort through research for information relevant to a research question. It familiarized me with the research process as I got to analyze the data from Dr. McCarty’s study. learned the amount of dedication, time, and careful effort that completing a research study requires by watching Dr. Dana McCarty with this project. The project made me a better clinician by improving my academic writing and editing skills. It increased my confidence in my ability to ask and answer clinically relevant questions by consulting literature. It gave me perspective on interdisciplinary care and patient management. This project also challenged my public speaking skills as I had to present to my fellow students and clinicians. Overall, this project challenged me and made me grow on a personal and professional level.
Acknowledgements
First and foremost, I would like to acknowledge and thank my advisor Dr. Dana McCarty. Dana devoted countless hours of time to meet via zoom, respond to emails, and counsel me throughout the creation of my products. I would also like to thank Shannon O’Donnell and Erika Clary for taking time out of their busy clinic schedules to be a part of my capstone committee. Without their endless support and direction this project would not have happened. I’d also like to thank all of the faculty in the DPT program for providing and excellent and fun formal education. Each of these clinicians motivates me to be a better clinician and further pursue formal and informal education opportunities in order to provide the highest quality care possible. I am extremely thankful for their support and input.
I’d also like to thank my two roommates Lexie and Jess for their endless support through all 3 years of PT school. From letting me practice on them for practical exams to making me coffee during late night cram sessions, they have been an unending source of support.
Lastly, I’d like to thank my fellow members of the 2021 DPT class. These past 3 years would have been agonizing without you all. Each one of you inspires me in some way to be a better and more active clinician. You have provided countless laughs, motivation, and support these past three years and I could not have done it without you all.
References
Bibliography
- Ifflaender S, Rüdiger M, Konstantelos D, Wahls K, Burkhardt W. Prevalence of head deformities in preterm infants at term equivalent age. Early Hum Dev. 2013;89(12):1041-1047. doi:10.1016/j.earlhumdev.2013.08.011
- Kunz F, Hirth M, Schweitzer T, et al. Subjective perception of craniofacial growth asymmetries in patients with deformational plagiocephaly. Clin Oral Investig. 2021;25(2):525-537. doi:10.1007/s00784-020-03417-y
- Vu GH, Magoon K, Zimmerman CE, et al. Perceptions and preferences of laypersons in the management of positional plagiocephaly. J Craniofac Surg. 2020;31(6):1613-1619. doi:10.1097/SCS.0000000000006524
- Pogliani L, Mameli C, Fabiano V, Zuccotti GV. Positional plagiocephaly: what the pediatrician needs to know. A review. Childs Nerv Syst. 2011;27(11):1867-1876. doi:10.1007/s00381-011-1493-y
- Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of Multiple Ventilation Courses and Duration of Mechanical Ventilation on Respiratory Outcomes in Extremely Low-Birth-Weight Infants. JAMA Pediatr. 2015;169(11):1011-1017. doi:10.1001/jamapediatrics.2015.2401
- Choi Y-B, Lee J, Park J, Jun YH. Impact of prolonged mechanical ventilation in very low birth weight infants: results from a national cohort study. J Pediatr. 2018;194:34-39.e3. doi:10.1016/j.jpeds.2017.10.042
- Williams E, Dassios T, Arnold K, Hickey A, Greenough A. Prolonged ventilation and postnatal growth of preterm infants. J Perinat Med. 2019;48(1):82-86. doi:10.1515/jpm-2019-0278
-
Saving Preemies | TIME. https://time.com/magazine/us/108686/june-2nd-2014-vol-183-no-21-u-s/. Accessed April 7, 2021.



2 Responses to “Neonatal Cranial Molding and Positioning Changes Related to Respiratory Device”
Dana B McCarty
Anna – well done! I enjoyed working with you and Ashley to bring this project to completion. I am so pleased with your voicethread and the graphics you created and presented. I am looking forward to getting this paper turned into a manuscript soon. Well done and congratulations!
Dana
Debbie Thorpe
Anna
Well done project. Very complete literature review and a great voice thread presentation! I learned some new information! The graphs in your presentation are very informative and add to understanding of conclusions. Good luck on poster acceptance!
Just a few editorial suggestions…check spelling through out and also complete this incomplete sentence” Ashely and I also collaborated during this time to create a poster with audio and submit to the…..?”
Good luck on the rest of your clinical rotations!
Best
Debbie