Heart Rate Variability and Exertional Task Analysis in the Recovery of Mild Traumatic Brain Injury in Service-Members (HEARTS)
A Comparison of Service-Members with mTBI and Healthy Service-Members
Katie Solheim, SPT
Background:
My experiences growing up as a military dependent, and more recently stepping into the role of an Army spouse, have greatly influenced my values and priorities in life. My desire to pursue a career in Physical Therapy was influenced by my aspirations to improve the health, well-being, and recovery of soldiers who have sustained injuries. Both the neuromuscular assessment and intervention course and the advanced neuromuscular intervention elective exposed me to traumatic brain injury (TBI) in civilian and military populations. Additionally, they provided me with a greater appreciation of how military training and activities inherent to the profession place service members at a much higher risk for this “silent” injury.
When presented with the opportunity to work under Karen McCulloch, PT, PhD, MS, FAPTA, NCS(E) on a study titled “Heart Rate Variability and Exertional Task Analysis in the Recovery of Mild Traumatic Brain Injury in Service Members” (HEARTS), I was eager to step into a role as a research assistant. HEARTS was started by a recent PhD graduate, Julianna Prim, PhD, for her dissertation project in the Department of Psychiatry, under the Human Movement Science Curriculum. She completed many of the preliminaries, to include collecting and analyzing data from the healthy control service member group. I was excited for the chance to engage with potential participants and be actively involved in data collection, as HEARTS is a non-funded project. Spending much of my childhood with my father stationed at Fort Bragg, NC, and my husband now stationed at this military instillation, I was thrilled to have the chance to interact with neuropsychologist, Wesley Cole, PhD, CBIS, who works in a clinical role at the Intrepid Spirit Center (ISC) on Fort Bragg. This clinic specializes in the treatment of traumatic brain injuries, or TBIs. I am very passionate about both neurologic physical therapy and the military community, and this capstone experience blended these two interests.
Statement of Need:
Between January 1 and December 18, 2020, the Department of Defense (DoD) reported 12,310 TBIs, with 10,546 being classified as mild.1 Concussions are prevalent in each branch of the military, in both stateside and deployment settings, related to service member operations, intensive training cycles, and leisure activities. Statistics are becoming more accurate with improved diagnostics and increased vigilance.1
The Department of Defense (DoD) states a mild traumatic brain injury (mTBI) or concussion is characterized by one of the following: “confused or disoriented state which lasts less than 24 hours; or loss of consciousness for up to 30 minutes; or memory loss lasting less than 24 hours.”2 Commonly experienced symptoms following a mTBI include dizziness, unsteadiness, trouble remembering, photophobia, phonophobia, headaches, fatigue, irritability, and confusion, but symptom sequalae varies based on both the injury and the individual.3 Current research indicates that “physiologic deficit” may persist even with self-report symptom resolution in the mTBI population. While the Defense and Veterans Brain Injury Center (DVBIC) has produced a guideline recommending exertional testing before making return to duty (RTD) decisions after a concussion, presently there are no specific standardized exercise tests that are clinically feasible and validated.4 Clinicians commonly determine duty readiness based on the absence of symptoms and return to “normal” performance on clinical assessment with ceiling effects.5 Additionally, a much greater amount of research has been devoted to making return to sport decisions in the child and adolescent age populations. While this information is valuable, decisions made in these specific populations cannot be directly extrapolated to the military. Research has indicated that military personnel often underreport symptoms, placing them at increased risk for premature RTD status with associated safety concerns.6 Additionally, a service member may have persistent physiological deficits after self-reported symptom improvement.7 Thusly, there is a need for the implementation of an objective physiologic measure, such as the assessment of heart rate variability (HRV), as a marker of autonomic dysfunction.8 HRV could be used to further evaluate exercise tolerance with tasks applicable to the military population in the subacute phase after a concussion. HEARTS has the potential to identify reliable, valid, and feasible performance-based tests with functional relevance, which could be routinely administered by a military primary care manager or rehabilitation provider.
Purpose and Clinical Relevance:
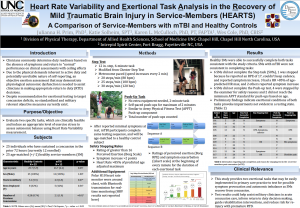
The overarching goal of this research is to improve assessment and management of acute concussion within the military health system. This study intends to investigate cardiac vagal control (CVC) in servicemembers with mTBI during rest, activity, and recovery phases of the protocol in the acute period post injury. The objective is to evaluate two specific exertional tests, a 6-minute step test and a 2-minute push up task, which are clinically feasible and induce an appropriate level of exercise stress to assess autonomic balance using Heart Rate Variability HRV) measurement. The findings from this study could help to fill gaps in acute concussion care in the military context, inform return to duty decision making, guide rehabilitation interventions, and minimize risk for re-injury with premature RTD.
Products:
During this capstone experience I was able to create an evidence table, write a preliminary abstract, compose a recruitment pitch and consent script, update the project flyer, and create a poster presentation for the UNC Department of Allied Health Sciences’ Interprofessional Research Fair.
I had the opportunity to participate in subject recruitment, enrollment, and data collection for this project on Fort Bragg at the Intrepid Spirit Center (ISC) between January 5th and February 26th during acute concussion clinic hours. I was able to formally test 5 subjects under the established protocol. Due to the unforeseen circumstances surrounding the COVID-19 pandemic we experienced several setbacks in being able to re-instate this research project in a timely manner at the ISC.
- Poster
- The main product of my capstone is an academic poster for the UNC Department of Allied Health Sciences’ Interprofessional Research Fair. This poster was submitted along with a brief presentation recording and describes the project protocol, background information on the topic, and preliminary findings from the service-members with concussion we have tested thus far.
- If you would like to view my presentation recording please follow this link and scroll to the bottom of the page.
- Preliminary Abstract
- This preliminary abstract was composed to be submitted with my poster presentation for the aforementioned virtual Interprofessional Research Fair.
- Evidence Table
- I created an evidence table to compile research on heart rate variability and exertional task analysis post-concussion to justify the need for this study and future research on concussion and return to activity, specific to the military population.
- Recruitment Flyer
- Cole and I updated the HEARTS recruitment flyer for providers at the Intrepid Spirit Center (ISC) to include more simplified wording with shorter statements and appropriate pictures. This flyer may be utilized as an “informational sheet” when providers are assessing a patient’s interest in participating in the study during acute concussion clinic appointments at the ISC.
- Recruitment Pitch and Consenting Script
- The creation of these products challenged me to consider simplifying sentence structure and language to make the recruiting and consenting processes easier to follow. It was critical I ensured participants thoroughly understood their rights as participants and what their involvement in the study would consist of, in terms of time commitment, paperwork, and task performance. It was also critical for me to verify participants understood the specific safety measures in place and recognized how their involvement in the study could impact the future care of soldiers who sustain concussions.
Evaluation:
My capstone advisor (Dr.McCulloch) and committee members provided guidance and feedback at each stage of my capstone project. Since this past summer I have engaged in several zoom video calls with these individuals to discuss how to move forward when we received updates regarding the status of the acute concussion clinic and transfer of the IRB. I was actively involved in group emails, texts, and calls. Dr. Prim took the time to shadow me the first time I tested an individual at the ISC, and my committee members were just as excited as I was when I consented my first participant and independently administered the testing protocol without supervision. Several times Dr. McCulloch thoughtfully devised a back-up plan when we were unsure we’d be able to start recruiting and enrolling at the ISC before my clinical rotation began. When prepping my recruiting pitch and consenting script my committee members took time out of their busy days to allow me to practice over zoom and receive direct feedback. I received ongoing feedback from Dr. McCulloch and Dr. Prim that guided me through the development of my abstract and poster presentation. I am actively seeking feedback from my classmates and community members regarding my academic research poster and presentation recording submitted to the Allied Health Sciences’ Interprofessional Research Fair. This feedback will be received through a short survey asking about the poster content and delivery of the presentation. It will be used to help appropriately modify the script and materials if the presentation is to be delivered again in the future.
Self-Reflection:
This experience exposed me to not only the challenges inherent to conducting research, but additionally the even greater challenges associated with conducting research during a Pandemic. I expressed my interest in the HEARTS study to Dr.McCulloch in May and in August 2020 I was trained by Julianna Prim, PhD, on the protocol for the study. Prior to actively becoming involved, Dr. Cole added me to the protocol and advised me on completing CITI training. In September the acute concussion walk-in clinic resumed, which was a huge step in the right direction, as the project was dependent upon the clinic resuming as the key source of recruitment. Around this time, we learned the IRB (Regional Health Command Atlantic) was disbanding and we were informed all protocols would be moved to Naval Medical Center Portsmouth (NMCP IRB). With this in mind we needed to adjust the consent to fit NMCP’s template. By November we finally got the modification and exception to policy though, meaning we could begin data collection. Unfortunately, with Thanksgiving and winter holiday leave for staff at the ISC and service members on Fort Bragg, I did not begin actively recruiting at the ISC until the first week of January. In the weeks leading up I was able to compose a recruitment pitch and consenting script. On February 4th Julianna drove down to Fort Bragg and met me at the ISC to run through the testing protocol (program and equipment set up) before I tested the first subject. I was able to participate in subject enrollment and data collection for this project on Fort Bragg at the Intrepid Spirit Center between January 5th and February 26th (between 7:30-9:30 am – acute concussion clinic hours). I was able to recruit and consent eight service members with mTBI, and formally test five of those individuals!
This capstone experience provided me with the opportunity to engage and build relationships with several of the military health care providers that specialize in the treatment of traumatic brain injury. I learned how to efficiently set up equipment and run the computer program for the study to collect HR data, and became more and more confident with each testing session. I safely implemented stopping rules for several of the subjects tested, due to elevated heart rate values. My committee members supported me in every way possible and I will be forever grateful for this experience!
Acknowledgments:
I would firstly like to thank Dr. Karen McCulloch, PT, PhD, FAPTA, NCS(E) for providing me with ongoing guidance and feedback throughout this capstone experience. I am extremely grateful for your plethora of insight on traumatic brain injuries in the military community and appreciate the mentorship you provided. Your enthusiasm and interest for working with individuals who have sustained TBIs and your dedication to the military community continues to inspire me!
Dr. Julianna Primm – Thank you for responding to my countless emails and texts and providing me with ongoing guidance on this topic. I appreciate your willingness to drive down to Fort Bragg to supervise me as I tested my first participant at the ISC.
Dr. Wes Cole – Thank you for making me feel welcomed at the ISC, for introducing me to all the providers, and for making room for me in the office.
Dr. Debbie Thorpe, PT, PhD – Thank you for facilitating the capstone project and providing guidance throughout.
Class of 2021 – I couldn’t be more grateful to have been surrounded by such supportive and encouraging peers over the last 3 years!
References:
- Traumatic Brain Injury Center of Excellence. Military Health System. https://health.mil/About-MHS/OASDHA/Defense-Health-Agency/Research-and-Development/Traumatic-Brain-Injury-Center-of-Excellence. Accessed April 5, 2021.
- Traumatic Brain Injury Center of Excellence (TBICoE). DoD Numbers for Traumatic Brain Injury Worldwide — Totals.
- VA research on Traumatic Brain Injury (TBI). U.S. Department of Veterans Affairs . https://www.research.va.gov/topics/tbi.cfm. Accessed April 11, 2021.
- Progressive Return to Activity Following Acute Concussion/Mild TBI Clinical Suite. DVBIC. https://dvbic.dcoe.mil/material/progressive-return-activity-following-acute-concussionmild-tbi-clinical-suite. Published March 19, 2020. Accessed April 10, 2021.
- Defense and Veterans Brain Injury Center. Concussion Management Tool. 2019.
- Gutierrez ML, Christy JB, Whitney SL. Development of Military Concussion Readiness Inventory for Dizziness and Balance. Patient Relat Outcome Meas. 2019;10:67-80. Published 2019 Feb 27. doi:10.2147/PROM.S171380
- Fino PC, Weightman MM, Dibble LE, et al. Objective Dual-Task Turning Measures for Return-to-Duty Assessment After Mild Traumatic Brain Injury: The ReTURN Study Protocol. Front Neurol. 2021;11:544812. Published 2021 Jan 15. doi:10.3389/fneur.2020.544812
- Bishop SA, Dech RT, Guzik P, Neary JP. Heart rate variability and implication for sport concussion. Clin Physiol Funct Imaging. 2018;38(5):733-742. doi:10.1111/cpf.12487
Photos from: USAToday (https://www.usatoday.com/story/news/nation-now/2015/08/10/army-celebrates-75-years-american-paratrooper/31404901/) and Army.mil (https://home.army.mil/bragg/index.php/my-fort-bragg/soldiers)



4 Responses to “Heart Rate Variability and Exertional Task Analysis in the Recovery of Mild Traumatic Brain Injury in Service-Members (HEARTS)”
Katie Solheim
Dr. Thorpe,
Thank you so much for taking the time to review my Capstone project. I learned so much from Kmac and my committee members. I enjoyed submitting my presentation to the DAHS IPE Research Fair and engaging in the synchronous Q&A! Thanks for all the guidance you provided throughout this capstone experience! -Katie
Debbie Thorpe
Katie
Fantastic job on this project!! Even with all the delays, you came through with a wonderful poster presentation that would be a great in service in the future and possible content for the neuro course with Kmac! Thank you for submitting to the DAHS IPE Research Fair and doing a great job of representing PT! Very professionally done. Your evidence table was very detailed and contained the latest evidence. You should be very proud of all the work you have one for this project. I thoroughly enjoyed reviewing it! Good luck on the rest of your clinical rotations!
Best
Debbie
Katie Solheim
Thank you Kmac!! This was a wonderful experience and I thoroughly enjoyed my time at the Intrepid Spirit Center. Thank you for your kind words and constant encouragement! The recruiting/consenting process taught me a great deal about the research process and participant testing was exciting! – Katie
Karen McCulloch
GREAT job on this project Katie – you did such good work to get things going again with recruitment – we are so grateful that you chose to make this a focus for your capstone. I hope that you have the opportunity to use your considerable skill and knowledge for military concussion with service members in the near future – they would benefit.
kmac