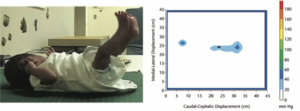
Picture Reference: Dusing, Kyvelidou, Mercer, Stergiou, 2009
Author: Jennifer Bosserman, SPT
Advisor: Dana McCarty, PT, DPT
Committee Members: Jessica Cassidy, PT, DPT, PhD and Kristen Dragotta PT, DPT
Background
Prior to beginning PT school, I already knew that I had a passion for pediatric physical therapy. I was able to further pursue this passion through our DPT curriculum, my time with children in the community, shadowing with Dana McCarty, PT, DPT, and my clinical rotation in early intervention. During my time in the Neonatal Intensive Care Unit (NICU) with Dana, I was able to observe infants with a wide variety of diagnoses including premature birth which furthered my interest in neonatal physical therapy. This experience combined with my early intervention clinical rotation caused me to consider how we can improve prognostic measurements for children early in their life to prevent future disability.
When Dana presented this project to me in the early Fall of 2022, I was excited to have the opportunity to complete research and create a manuscript focused on improving prognosis and encouraging early treatment for children with potential motor impairments. Throughout the fall I created a focused research question, came up with inclusion and exclusion criteria, completed a thorough literature search, data extraction, and quality assessment for the chosen literature on this topic. I have been able to complete a manuscript as my capstone this semester that not only expanded my knowledge on postural control in preterm infants, but also describes how therapists can utilize this information to minimize motor impairment and disability in the future.
Statement of Need
There is a risk of motor impairment in all preterm infants born at <37 weeks gestation, however, the risk is highest in infants born moderately preterm (32-34 weeks gestation) at 20.6% and very preterm (<32 weeks gestation) at 36.1%.1,2 Risk of motor impairment in full-term infants ranges from 2-7% compared to 54-64% in preterm infants and there are notable differences in the movement patterns of preterm infants as compared to full-term infants.3 Further, preterm infants are more likely to display body and head asymmetry and show preference for extension patterns than full-term infants.6
Current evidence supports parent and therapist delivered motor intervention to improve motor and cognitive development and outcomes in preterm infants,18 and immediate, ongoing therapy services after hospital discharge to reduce the risk of developmental delays; however, there is often a delay in therapy services after NICU discharge,19,20 especially if no significant motor impairment or diagnosis is documented using a standardized or objective measure. The increased risk for developmental impairment in preterm infants demonstrates the need for a measure for future motor delay in order to provide timely, appropriate therapy services.
In the absence of extended time for clinicians to attend training programs and funding to pay for such programs, it is prudent to identify objective measures that indicate potential delay that can be used, assessed, and understood by a variety of clinicians and researchers. Quantitative measurements such as center of pressure (COP) and variability of movement have been shown to be predictive of motor impairment or delay in preterm infants,24 but these measures are not currently used in the clinical setting to identify infants at risk for movement delay.
Purpose
This study aimed to meet the needs listed above. The purpose of this manuscript was to evaluate the existing evidence regarding the use of pressure mats or force plates to measure postural control and movement in preterm infants. We also evaluated how those measures differ in preterm and full-term infants and how these differences may predict future motor impairment or disability in this population.
Products
To begin, I completed an initial keyword search which identified nine hundred articles. Full-text review for eligibility was completed for twenty-five full text studies, and eight met all eligibility criteria. I then used this literature to create my systematic review with Dana’s assistance which we will be submitting for publication to an academic journal. This manuscript discusses the use of pressure mats and force plates to assess postural control, and further utilize this information to determine likelihood of future motor impairment in preterm infants.
Evaluation and Self Reflection
Materials were delivered to all committee members and are being prepared to submit to an academic journal for publishing. I received feedback from my committee members who are pediatric physical therapists and also research specialists about the quality of my project. I feel as though I still have much progress to be made regarding my research skills but have met all of my learning objectives for this project. I have grown tremendously under the mentorship of my advisor Dana and also my committee members Kristen and Jessica. I plan to also submit and present this research at CSM in 2024 and have created an evaluation sheet to assess the understanding of the topic and also my presentation techniques.
Evaluation-Form-
Acknowledgements
To Dana McCarty, PT, DPT thank you so much for your support throughout this project and also my time here at UNC. You have not only been a great mentor in my journey of physical therapist, but you have also showed me what a great pediatric clinician looks like. Your passion and dedication for pediatrics is something that I hope to emulate within myself. You have been such an impact in helping me reach my goals as a pediatric physical therapist and I cannot thank you enough for that.
To Jessica Cassidy, PT, DPT, PhD, thank you for agreeing to be on my capstone committee and for all of your valuable feedback throughout this process. Your research experience and excellence was a large help while completing my manuscript. I am very appreciative of all of your assistance with this project but also throughout my journey here at UNC.
To Kristen Dragotta, PT, DPT, thank you for agreeing to serve on my capstone committee with all that you have going on with your life and career. I am very appreciative of the time you took to review my work and provide me with insightful feedback based on your experience in the NICU.
References
1. Van Hus JW, Potharst ES, Jeukens-Visser M, Kok JH, Van Wassenaer-Leemhuis AG. Motor impairment in very preterm-born children: links with other developmental deficits at 5 years of age. Dev Med Child Neurol. 2014;56(6):587-594. doi:10.1111/dmcn.12295
2. Bélanger R, Mayer-Crittenden C, Minor-Corriveau M, Robillard M. Gross Motor Outcomes of Children Born Prematurely in Northern Ontario and Followed by a Neonatal Follow-Up Programme. Physiother Can. 2018;70(3):233-239. doi:10.3138/ptc.2017-13
3. More preemies developing motor impairments | Reuters. Accessed March 28, 2023. https://www.reuters.com/article/us-health-preemies-motor-impairments/more-preemies-developing-motor-impairments-idUSKBN1GY29D
4. Kakebeeke TH, von Siebenthal K, Largo RH. Movement quality in preterm infants prior to term. Biol Neonate. 1998;73(3):145-154. doi:10.1159/000013971
5. Fjørtoft T, Evensen KAI, Øberg GK, et al. High prevalence of abnormal motor repertoire at 3 months corrected age in extremely preterm infants. Eur J Paediatr Neurol. 2016;20(2):236-242. doi:10.1016/j.ejpn.2015.12.009
6. Örtqvist M, Einspieler C, Marschik PB, Ådén U. Movements and posture in infants born extremely preterm in comparison to term-born controls. Early Hum Dev. 2021;154:105304. doi:10.1016/j.earlhumdev.2020.105304
7. Dusing SC, Izzo TA, Thacker LR, Galloway JC. Postural complexity differs between infant born full term and preterm during the development of early behaviors. Early Hum Dev. 2014;90(3):149-156. doi:10.1016/j.earlhumdev.2014.01.006
8. de Groot L, Hopkins B, Touwen B. Motor asymmetries in preterm infants at 18 weeks corrected age and outcomes at 1 year. Early Hum Dev. 1997;48(1-2):35-46. doi:10.1016/s0378-3782(96)01796-3
9. de Groot L. Posture and motility in preterm infants. Dev Med Child Neurol. 2000;42(1):65-68. doi:10.1017/s0012162200000128
10. Williams KG, Patel KT, Stausmire JM, Bridges C, Mathis MW, Barkin JL. The Neonatal Intensive Care Unit: Environmental Stressors and Supports. Int J Environ Res Public Health. 2018;15(1):60. Published 2018 Jan 3. doi:10.3390/ijerph15010060
11. Sweeney JK, Gutierrez T. Musculoskeletal implications of preterm infant positioning in the NICU. J Perinat Neonatal Nurs. 2002;16(1):58-70. doi:10.1097/00005237-200206000-00007
12. Byrne E, Garber J. Physical therapy intervention in the neonatal intensive care unit. Phys Occup Ther Pediatr. 2013;33(1):75-110. doi:10.3109/01942638.2012.750870
13. Nuysink J, van Haastert IC, Eijsermans MJC, et al. Prevalence and predictors of idiopathic asymmetry in infants born preterm. Early Hum Dev. 2012;88(6):387-392. doi:10.1016/j.earlhumdev.2011.10.001
14. Dunsirn S, Smyser C, Liao S, Inder T, Pineda R. Defining the nature and implications of head turn preference in the preterm infant. Early Hum Dev. 2016;96:53-60. doi:10.1016/j.earlhumdev.2016.02.002
15. Konishi Y, Mikawa H, Suzuki J. Asymmetrical head-turning of preterm infants: some effects on later postural and functional lateralities. Dev Med Child Neurol. 1986;28(4):450-457. doi:10.1111/j.1469-8749.1986.tb14282.x
16. Pierrat V, Marchand-Martin L, Arnaud C, et al. Neurodevelopmental outcome at 2 years for preterm children born at 22 to 34 weeks’ gestation in France in 2011: EPIPAGE-2 cohort study. BMJ. 2017;358:j3448. Published 2017 Aug 16. doi:10.1136/bmj.j3448
17. Seaton SE, Barker L, Draper ES on behalf of the UK Neonatal Collaborative, et alEstimating neonatal length of stay for babies born very pretermArchives of Disease in Childhood – Fetal and Neonatal Edition 2019;104:F182-F186.
18. Khurana S, Kane AE, Brown SE, Tarver T, Dusing SC. Effect of neonatal therapy on the motor, cognitive, and behavioral development of infants born preterm: a systematic review. Dev Med Child Neurol. 2020;62(6):684-692. doi:10.1111/dmcn.14485
19. McManus BM, Richardson Z, Schenkman M, Murphy N, Morrato EH. Timing and Intensity of Early Intervention Service Use and Outcomes Among a Safety-Net Population of Children. JAMA Netw Open. 2019;2(1):e187529. Published 2019 Jan 4. doi:10.1001/jamanetworkopen.2018.7529
20. Nwabara O, Rogers C, Inder T, Pineda R. Early Therapy Services Following Neonatal Intensive Care Unit Discharge. Phys Occup Ther Pediatr. 2017;37(4):414-424. doi:10.1080/01942638.2016.1247937
21. Wang J, Siddicky SF, Johnson T, Kapil N, Majmudar B, Mannen EM. Supine lying center of pressure movement characteristics as a predictor of normal developmental stages in early infancy. Technol Health Care. 2022;30(1):43-49. doi:10.3233/THC-202754
22. Noble Y, Boyd R. Neonatal assessments for the preterm infant up to 4 months corrected age: a systematic review. Dev Med Child Neurol. 2012;54(2):129-139. doi:10.1111/j.1469-8749.2010.03903.x
23. Pineda R, McCarty DB, Inder T. Neurological and Neurobehavioral Evaluation. In: Inder T, ed. Neonatology Questions and Controversies. In Press.
24. Prosser LA, Aguirre MO, Zhao S, et al. Infants at risk for physical disability may be identified by measures of postural control in supine. Pediatr Res. 2022;91(5):1215-1221. doi:10.1038/s41390-021-01617-0
25. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467-473. doi:10.7326/M18-0850
26. Bosserman J. Can Center of Pressure Measurement Predict Future Motor Impairment in Preterm Infants: A Systematic Review. osf.io/28afw. Published October 27, 2022.
27. Veritas Health Innovation. Covidence systematic review software. Date Unknown. Computer software, Veritas Health InnovatioMelbourne, Australia.
28. Rethlefsen ML, Page MJ. PRISMA 2020 and PRISMA-S: common questions on tracking records and the flow diagram. J Med Libr Assoc. 2022;110(2):253-257. doi:10.5195/jmla.2022.1449
29. Chapter 5: Collecting data | Cochrane Training. Accessed November 29, 2022. https://training.cochrane.org/handbook/current/chapter-05
30. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898.
31. Dusing SC, Thacker LR, Galloway JC. Infant born preterm have delayed development of adaptive postural control in the first 5 months of life. Infant Behav Dev. 2016;44:49-58. doi:10.1016/j.infbeh.2016.05.002
32. Fallang B, Hadders-Algra M. Postural behavior in children born preterm. Neural Plast. 2005;12(2-3):175-272. doi:10.1155/np.2005.17
33. Fallang, B., Øien, I., Hellem, E. et al. Quality of Reaching and Postural Control in Young Preterm Infants Is Related to Neuromotor Outcome at 6 Years. Pediatr Res 58, 347–353 (2005). https://doi.org/10.1203/01.PDR.0000170898.60160.09
34. Dusing SC, Kyvelidou A, Mercer VS, Stergiou N. Infants born preterm exhibit different patterns of center-of-pressure movement than infants born at full term. Phys Ther. 2009;89(12):1354-1362. doi:10.2522/ptj.20080361
35. Dusing S, Mercer V, Yu B, Reilly M, Thorpe D. Trunk position in supine of infants born preterm and at term: an assessment using a computerized pressure mat. Pediatr Phys Ther. 2005;17(1):2-10. doi:10.1097/01.pep.0000154106.52134.80
36. Dusing SC, Izzo T, Thacker LR, Galloway JC. Postural complexity influences development in infants born preterm with brain injury: relating perception-action theory to 3 cases. Phys Ther. 2014;94(10):1508-1516. doi:10.2522/ptj.20140023
37. State of New Mexico, New Mexico. Accessed January 27, 2023. https://newmexico.networkofcare.org/aging/assistive/detail.aspx?id=13393&cid=0&cn=&org=vista-medical-ltd
38. Delgado-Bonal, A., & Marshak, A. (2019). Approximate Entropy and Sample Entropy: A Comprehensive Tutorial. Entropy (Basel, Switzerland), 21(6), 541. https://doi.org/10.3390/e21060541
39. Palmieri RM, Ingersoll CD, Stone MB, Krause BA. Center-of-Pressure Parameters Used in the Assessment of Postural Control. J Sport Rehabil. 2002;11(1):51-66. doi:10.1123/jsr.11.1.51
40. Vaivre-Douret L, Ennouri K, Jrad I, Garrec C, Papiernik E. Effect of positioning on the incidence of abnormalities of muscle tone in low-risk, preterm infants. Eur J Paediatr Neurol. 2004;8(1):21-34. doi:10.1016/j.ejpn.2003.10.001
41. Seating Design & Testing | Wheelchair Pressure Mapping | CONFORMat System | Tekscan. Accessed January 27, 2023. https://www.tekscan.com/products-solutions/systems/conformat-system
42. Motion – What is Motion, Difference Between Path Length and Displacement, Video and FAQs. Accessed January 27, 2023. https://byjus.com/physics/position-path-length-displacement/
43. Biomechanics and life sciences | Kistler. Accessed January 27, 2023. https://www.kistler.com/INT/en/biomechanics-and-life-sciences/C00000187
44. AMTI – Multi-Axis Force Sensors | Accuracy Matters. Accessed January 27, 2023. https://www.amti.biz/
45. Center of Pressure – Glenn Research Center | NASA. Accessed January 27, 2023. https://www1.grc.nasa.gov/beginners-guide-to-aeronautics/center-of-pressure/
46. Dusing SC, Tripathi T, Marcinowski EC, Thacker LR, Brown LF, Hendricks-Muñoz KD. Supporting play exploration and early developmental intervention versus usual care to enhance development outcomes during the transition from the neonatal intensive care unit to home: a pilot randomized controlled trial. BMC Pediatr. 2018;18(1):46. Published 2018 Feb 9. doi:10.1186/s12887-018-1011-4
47. Örtqvist M, Marschik PB, Toldo M, et al. Reliability of the Motor Optimality Score-Revised: A study of infants at elevated likelihood for adverse neurological outcomes [published online ahead of print, 2023 Mar 9]. Acta Paediatr. 2023;10.1111/apa.16747. doi:10.1111/apa.16747
48. Kniaziew-Gomoluch K, Szopa A, Kidoń Z, Siwiec A, Domagalska-Szopa M. Design and Construct Validity of a Postural Control Test for Pre-Term Infants. Diagnostics (Basel). 2022;13(1):96. Published 2022 Dec 29. doi:10.3390/diagnostics13010096
49. Sec. 303.1 Purpose of the early intervention program for infants and toddlers with disabilities – Individuals with Disabilities Education Act. Accessed July 8, 2022. https://sites.ed.gov/idea/regs/c/a/303.1
50. Byrne E, Campbell SK. Physical therapy observation and assessment in the neonatal intensive care unit. Phys Occup Ther Pediatr. 2013;33(1):39-74.

7 Responses to “Postural Control Measurements to Predict Future Motor Impairment in Preterm Infants”
sarahjmc
Jenny,
Your Capstone and manuscript (future publication) are amazing. Getting to pioneer in this field of research is a big deal and extremely important. The only way to provide improvements in these developmental delays is to do the work that you are doing. I am so proud of your hard work, great attitude, and joy in doing this work. You are going to make an incredible PT and educator, and I look forward to seeing the work that you will do in the future. Wonderful job!!
Sarah
kallysaf
Jenny,
You did such an incredible job with this project! It is obvious how much work you put into this, and how passionate you are about pediatric physical therapy. Even for somebody who is not necessarily interested in pediatric therapy, I got so much out of this project and know that it will play a role in decrease the disability and motor deficit in future patients. I cannot wait to see you do amazing things!
Megna Mishra
Jenny,
I am so proud of you! I’ve witnessed firsthand the passion, thought, hard work, and time you’ve put into this project. It’s been so fun to see you dive into the research and the research world in general. I already knew you were a great peds therapist, but now after this, you are great peds researcher too! I’m so happy for you and all that you’ve accomplished. You are so deserving of this and I can’t wait to come visit you when you present this at CSM!
Vicki Mercer
Jennifer – Excellent work! This is a great start to what I am sure will be a long list of contributions to pediatric physical therapy!
I’m also glad to see that Stacey Dusing’s early research projects (done here at UNC) still have relevance.
Dana B McCarty
Jenny – You went above and beyond my expectations and created a very strong manuscript that will contribute to the body of knowledge for pediatric therapists! I am excited about what you have accomplished and can’t wait to see what you do in the peds world!
Jessica Cassidy
Jennifer- Fantastic work and thoughtful reflection. I’m excited that you’re planning to both publish this work and submit it to CSM 2024. You should feel very proud. Congratulations.
Megna Mishra
Jenny,
I am so proud of you! I’ve witnessed firsthand the thought, time, effort, and enthusiasm you put into this project. I’m so happy that you loved this research part of practice. I already knew you were a great peds therapist, but now I know you are also a great peds researcher! I’m so proud of you and all your hard work! You are so deserving! Now go change the world!! Can’t wait to see this at CSM in the future (I will humble brag the whole time don’t you worry).