Predictors of Cranial Molding Deformities in Preterm Infants
By: Sonia Kelkar, SPT

Background
Since starting in the Doctor of Physical Therapy program at UNC-Chapel Hill, I have always known that I had an interest in working with the pediatric population. This interest has only grown stronger in the past 3 years, based on our coursework, lab experiences, and a clinical rotation in pediatric acute care. I love the opportunity to work with patients with a variety of presentations and conditions, including orthopedic, neurological, genetic, cardiopulmonary, and oncological. Additionally, I enjoy the challenge of making each intervention fun and exciting for patients.
During my third clinical rotation at UNC Children’s Hospital, I was first exposed to the Neonatal Intensive Care Unit, as both my clinical instructors, Kerry Blazek, PT, DPT, and Kristen Dragotta, PT, DPT, treated patients in this setting. Physical therapy in the NICU is quite different to anything else we have learned about. I was very intrigued to learn how PTs can help to support the development of these very tiny infants, who were born as early as 22 weeks gestational age.
Towards the end of my rotation, I learned about the research project that Dana McCarty, PT, DPT, was working on. I immediately knew that I wanted to work alongside her, as part of my research elective. Dana wanted to examine how respiratory support in the NICU might contribute to the development of abnormal cranial molding, among preterm infants. For my research elective, I learned how to take head measurements of infants in the NICU, using orthopedic cranial calipers. Using this data, we were able to examine how head shape is related to respiratory support and various other variables in preterm infants.
Statement of Need and Purpose
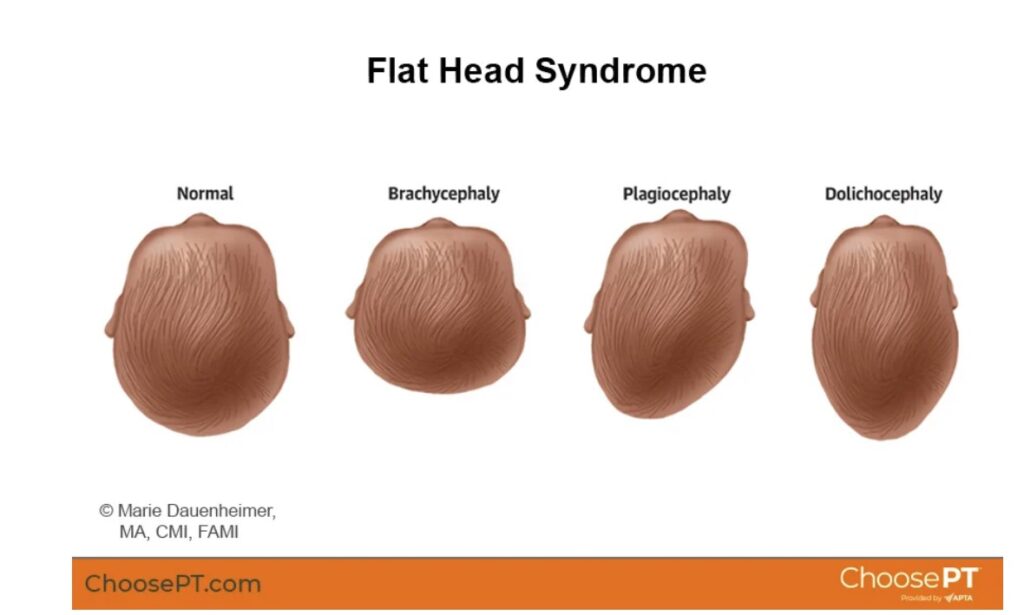
Preterm birth is very common in the United States, with 1 out of every 10 infants born before 37 weeks gestation. Preterm birth puts infants at a higher risk of a variety of issues including respiratory distress syndrome, intraventricular hemorrhage (IVH), and developmental delay. 1 They are also at a higher risk of cranial molding deformities, due to low muscle tone, difficulty moving against gravity, and abnormal movement and postural patterns.2–5 Dolichocephaly, specifically, is not well studied, but tends to occur most often in preterm infants, due to difficulty maintaining the head in midline against the effects of gravity and prolonged sidelying positioning. This results in the infant resting with the head rotated to either side, causing flattening of the lateral skull bilaterally.6 Plagiocephaly, an asymmetrical deformity, is also highly prevalent in preterm infants.2,7
While there have been many studies into the high prevalence of cranial molding deformities in preterm infants, the literature around predictors of these deformities and ways to prevent them is still limited. Preterm infants often require respiratory interventions such as mechanical ventilation or continuous positive airway pressure (CPAP), which limit their movements and requires prolonged positioning with the head in one position.2 Additionally, the pressure caused by the attachments and caps used with CPAP devices may also contribute to abnormal cranial molding, as they require a tight fit in order to function properly.

As respiratory distress syndrome is the most common complication for premature infants, and CPAP is a common treatment, it is important that we understand how this treatment can contribute to cranial molding.8 Furthermore, once these deformities develop, infants are at a higher risk of delayed gross motor, language, and cognitive development, and asymmetrical movement patterns.9–12 Therefore, it is important for us to understand the causes of cranial molding deformities and the best way to prevent and treat them.
Purpose
The purpose of this study was to determine if there is a correlation between days spent on CPAP and the severity of asymmetrical and symmetrical head deformities, among preterm infants. For this study, we took head measurements of 20 preterm infants hospitalized in the Neonatal Critical Care Unit at UNC Children’s Hospital between August 2022 and February 2023. Infants were included based on the following criteria: birth gestational age ≤32 weeks and stable on room air, low-flow nasal cannula, or high-flow nasal canula, at the time of measurement. We also collected demographic data including birth gestational age, current gestational age, days on CPAP, days on mechanical ventilation, diagnosis of interventricular hemorrhage (IVH) and grade, and documentation of asymmetry by PT or OT in the week prior to the measurement. Additionally, comorbidity count, which includes the presence of bronchopulmonary dysplasia (BPD) or chronic lung disease (CLD), severe IVH, severe retinopathy of prematurity (ROP), and any infection during hospitalization, was recorded for each patient.
Products
The main products of this study were designed to display the results of our study. I created a poster presentation of our findings. I also wrote an abstract, which we will be submitting to a physical therapy conference in the next year, for a poster or podium presentation:
Cranial Molding and Preterm Infants Abstract
Predictors of Cranial Molding Deformities in Preterm Infants Poster
I also conducted a literature review of the prevalence, prevention and treatment of cranial molding deformities in preterm infants. I summarized the findings of 11 articles in the following evidence table:
Lastly, I created a caregiver education handout, which describes plagiocephaly and dolichocephaly, explains what causes them, and provides information on prevention and treatment. This handout was created to serve as a supplement to verbal education that we often provided, when caregivers were present when we arrived at the bedside for head measurements. This would allow caregivers to have a written document to refer back to, in case they did not remember everything that we explained to them verbally. Additionally, the handout provides concrete examples of things that are currently being done to prevent abnormal cranial molding, as well as things that they can do on their own once their child is discharged.
Health Literacy
Low health literacy is a common issue in the United States. The National Assessment of Adult Literacy (NAAL) which was last conducted in 2003 found that only 12% of adults had proficient levels of health literacy, while 22% of adults had basic levels and 14% had below basic levels of health literacy.13 Low health literacy among caregivers of pediatric patients is associated with poorer child health outcomes.14 Specifically, in the NICU, as many as 43% of parents of infants in the NICU were found to have suspected low health literacy at admission.15
When creating my caregiver education handout, I wanted to make it readable and understandable to any caregiver. I tried to avoid the use of medical jargon in the handout and kept sentences short and simple. I also tried to use positive language, to keep the tone of the handout encouraging for caregivers. Visually, I used a light background with dark text, which is easy to read. I avoided the use of lengthy paragraphs, and used bulleted lists when appropriate.16 I aimed to maintain a 4th-6th grade reading level. I used Fry’s Readability Index to measure the reading level. This index looks at the number of syllables and number of sentences in a 100-word sample. In order to maintain a lower reading level, the sample should have fewer syllables and fewer sentences.17
I evaluated 2 100-word samples from the handout to ensure that the reading level was appropriate.
Sample 1:
Syllables: 143
Sentences: 8
Grade Level: 5th – 6th grade
Sample 2:
Syllables: 134
Sentences: 9.25
Grade Level: 5th grade
Evaluation Component:
I have been receiving feedback from my advisor, Dana McCarty and my committee members, Kerry Blazek and Catherine Cunningham during the semester. I met with Dana several times throughout the semester to discuss the results of my data and my capstone products. Based on these discussions, I was able to pinpoint the most important data points from our results, which are presented in the poster. Additionally, I received helpful feedback from my committee on my capstone products. In particular, they were able to provide helpful insight on my caregiver education handout, and advised me on relevant details that would be of interest to caregivers.
I have also created two evaluation forms for my products, one for the poster and a second for the caregiver education handout.
Poster: https://forms.gle/rdLDw6xFhseXbK6C7
Handout: https://forms.gle/U2CJ7UrYx6YeVxJF6
Self-Assessment:
Working on my research project and capstone has been a great opportunity for growth over the past year. Overall, I have been able to meet the objectives I set for myself. I have been able to learn so much about neonatal physical therapy in general, as well as the specifics of cranial molding deformities. Furthermore, this year, I have been able to further explore my interest in research. Prior to PT school, I worked for a research lab, primarily working on retrospective research projects, in which we analyzed data from thousands of patients. This year, I have gained a better understanding of what it is like to conduct research prospectively in a clinical setting. We spent over 7 months collecting data for the 20 patients included in our study, and we often had to contend with the challenges of conducting research on subjects who are currently inpatient, such as changes in medical status or scheduling issues.
I also feel that my skills in literature review have improved considerably. There is a lack of research on neonatal physical therapy, which required me to really hone my search skills and comb through the literature to find what I needed. Additionally, I have been able to work on writing skills, for various audiences. I have created a poster and written an abstract, which has allowed me to display the results of our work over the past year to clinicians, students, and other healthcare providers. Additionally, I created a handout aimed at caregivers and parents, which required me to work on presenting medical information in a manner than can be understood by individuals without a medical background. Both of these types of writing are challenging for me, so I am glad that I had the opportunity to practice both, with the guidance of my capstone advisor and committee members.
One thing that I would have liked to do as part of this project was submit my abstract to the UNC Human Movement Science Research Symposium, as it would have been a great opportunity to present our work to others at UNC. Unfortunately, due to the time we completed our data collection, we were not prepared to meet the submission deadline. However, I am excited to be submitting my abstract for consideration to physical therapy conference such as CSM, and hope to be able to present this research at a conference in the future.
Overall, I am really proud of everything that I have accomplished over the past year. I have always had an interest in research, and this year has helped me grow my research skills. Whether I continue to do any type of research in my career or not, I know that I will be able to use these skills for evidence-based practice!
Acknowledgements:
Thank you to Dana McCarty, PT, DPT, for giving me the opportunity to work on this project with you. You have provided me with so much guidance and expertise over the past year, which has really contributed to the success of this project. I appreciate all of the time you have spent helping me to make this project what it is.
Thank you to my capstone committee members, Kerry Blazek, PT, DPT, and Catherine Cunningham, PT, DPT, for agreeing to be on my capstone committee! I really appreciate the time you took out of your busy schedules to provide me with valuable feedback on my capstone products.
Thank you to the Class of 2023, for a wonderful 3 years! Starting PT school in the middle of a pandemic was definitely a rollercoaster, but we made it! I can’t wait to see all that we accomplish in the years to come!
Bibliography
- Preterm Birth | Maternal and Infant Health | Reproductive Health | CDC. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm. Accessed April 21, 2023.
- Ifflaender S, Rüdiger M, Konstantelos D, Wahls K, Burkhardt W. Prevalence of head deformities in preterm infants at term equivalent age. Early Hum Dev. 2013;89(12):1041-1047. doi:10.1016/j.earlhumdev.2013.08.011
- Örtqvist M, Einspieler C, Marschik PB, Ådén U. Movements and posture in infants born extremely preterm in comparison to term-born controls. Early Hum Dev. 2021;154:105304. doi:10.1016/j.earlhumdev.2020.105304
- Franki I, Bar-On L, Molenaers G, et al. Tone Reduction and Physical Therapy: Strengthening Partners in Treatment of Children with Spastic Cerebral Palsy. Neuropediatrics. 2020;51(2):89-104. doi:10.1055/s-0039-3400987
- Miyagishima S, Asaka T, Kamatsuka K, et al. Characteristics of antigravity spontaneous movements in preterm infants up to 3 months of corrected age. Infant Behav Dev. 2016;44:227-239. doi:10.1016/j.infbeh.2016.07.006
- McCarty DB, Peat JR, Malcolm WF, Smith PB, Fisher K, Goldstein RF. Dolichocephaly in preterm infants: prevalence, risk factors, and early motor outcomes. Am J Perinatol. 2017;34(4):372-378. doi:10.1055/s-0036-1592128
- Nuysink J, van Haastert IC, Eijsermans MJC, et al. Prevalence and predictors of idiopathic asymmetry in infants born preterm. Early Hum Dev. 2012;88(6):387-392. doi:10.1016/j.earlhumdev.2011.10.001
- Yadav S, Lee B, Kamity R. Neonatal respiratory distress syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
- Collett BR, Kartin D, Wallace ER, Cunningham ML, Speltz ML. Motor Function in School-Aged Children With Positional Plagiocephaly or Brachycephaly. Pediatr Phys Ther. 2020;32(2):107-112. doi:10.1097/PEP.0000000000000687
- Collett BR, Wallace ER, Ola C, Kartin D, Cunningham ML, Speltz ML. Do Infant Motor Skills Mediate the Association Between Positional Plagiocephaly/Brachycephaly and Cognition in School-Aged Children? Phys Ther. 2021;101(2). doi:10.1093/ptj/pzaa214
- Collett BR, Starr JR, Kartin D, et al. Development in toddlers with and without deformational plagiocephaly. Arch Pediatr Adolesc Med. 2011;165(7):653-658. doi:10.1001/archpediatrics.2011.92
- McCarty D, Hyams M. Fact Sheet: Considerations for Cranial Molding in the Neonatal Intensive Care Unit. APTA Academy of Pediatric Physical Therapy. https://pediatricapta.org/includes/fact-sheets/pdfs/FactSheet_ConsidersationsforCranialMoldingNICU_2022.pdf?v=1. Published 2022. Accessed April 3, 2023.
- Kutner M, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006-483. National Center for education statistics. 2006.
- Lawrence PR, Feinberg I, Spratling R. The Relationship of Parental Health Literacy to Health Outcomes of Children with Medical Complexity. J Pediatr Nurs. 2021;60:65-70. doi:10.1016/j.pedn.2021.02.014
- Mackley A, Winter M, Guillen U, Paul DA, Locke R. Health literacy among parents of newborn infants. Adv Neonatal Care. 2016;16(4):283-288. doi:10.1097/ANC.0000000000000295
- Office of Communication Centers for Disease Control and Prevention. Simply Put: A guide for creating easy-to-understand materials. April 1999.
- Schrock K. Fry’s Readability Information . Kathy Schrock’s Guide to Everything. https://www.schrockguide.net/frys-readability-info.html. Accessed May 29, 2022.

One Response to “Predictors of Cranial Molding Deformities in Preterm Infants”
Dana B McCarty
Sonia – you managed a Capstone project with lots of components and moving pieces. You stayed on top of it and pulled it all together beautifully. I am really proud of the work you’ve done here!