Understanding Bowel, Bladder and Sexual Function in a Neurologic Population: The Role of the Physical Therapist
Sarah Richardson, SPT
Background:
Since very early on, I have found myself interested in pursuing Women’s Health and pelvic floor physical therapy upon graduation. However, following the completion of the Neuromuscular Intervention I and II coursework, I recognized that there appeared to be a gap in the understanding and management of secondary bowel, bladder, and sexual dysfunction in patients with neurologic conditions. Given my passion for women’s health, I became curious about what role physical therapists could play in the management of bowel, bladder, and sexual function in neurological populations. This inquiry led me to take a course offered by Herman & Wallace titled, “Parkinson Disease and Pelvic Rehabilitation” which outlined how pelvic floor physical therapists can evaluate and treat neurologically complex patients. With this newfound knowledge, I wanted to bring this information to the curriculum within the Neuromuscular Intervention course series and thought my capstone would be the perfect opportunity to achieve this. I reached out to Karen McCulloch and Vicki Mercer, the professors of the Neuromuscular Intervention Courses, with my idea to adapt and update the online self-study unit within the spinal cord injury curriculum that discussed bowel, bladder, and sexual functioning. This conversation was the catalyst for my project and now, I am humbled to be able to share my Capstone website with you all and to present the culmination of my hard work.
Statement of Need:
Individuals who sustain spinal cord injuries can experience secondary bowel, bladder, and sexual dysfunction, which is a common sequela reported in this patient population. It’s even been found that patients who endure a spinal cord injury most consistently mention issues related to bowel and bladder problems and pain.1 However, this high prevalence of concern doesn’t always translate to adequate care. Studies have found that the journey of care is challenging for persons with spinal cord injury, their care providers, and community-based advocates.2 Although patients recognize their role in decision making, this is not always the case.3 Qualitative studies have found that many patients feel that the “doctors know best” and some even report that doctors override their own health care decision, impacting their sense of autonomy.3 Health professionals need to educate patients about disease and treatment options and allow patients to express their preferences and degree of comfort prior to selecting an option regardless of age, injury severity, and level of dependency.3
Although physical therapists are not directly involved in the decision-making process for neurogenic bowel or bladder management, they can play a vital role in advocacy, patient education, and promoting functional positions that make bladder and bowel management more successful. For example, “physical therapy can have a positive effect on a bladder management program by maximizing a patient’s wheelchair mobility”.4 In some physical therapy specialties, such as Women’s Health, there are additional conservative treatment approaches for this patient population including pelvic floor muscle training, body-weight supported treadmill walking, and electrical stimulation.5–8 If therapists have a greater understanding of the impact of a spinal cord injury on these systems, then they are better equipped to make appropriate referrals, provide relevant patient education, and create functional goals that complement a patient’s bladder or bowel management program. The Neuromuscular II – PT Intervention Course (PHYT 785) within the University of North Carolina’s Doctor of Physical Therapy program historically has included an online learning unit covering this topic with a complementary quiz. However, based on conversations with classmates and the professors of this course, there appears to be a common misunderstanding of the course material as well as the role of a physical therapist in addressing this sequela in patients with spinal cord injury. Given the significant impact that a spinal cord injury can have on these functions and the subsequent impact that dysfunction can have on one’s quality of life, students pursuing a career in physical therapy must have a clear understanding of this sequela and their role in management.
Upon graduation, I hope to work with this patient population and enhance the non-surgical and non-pharmacological options available for the management of this sequela. That is why I decided to adapt the Online Self-Study Unit in PHYT 785 that discusses bowel, bladder, and sexual function following a spinal cord injury so that I could educate current physical therapy students as to the role they play for this patient population. Empowering future physical therapy students to feel confident in their understanding of this patient population and how to best care for them is a professional goal of mine.
Overview & Purpose:
This capstone intends to update the current online self-study unit within the PHYT 785 course to reflect the most up-to-date research on this patient population. By expanding the current online unit, I hope to clarify the impact of a spinal cord injury on bladder, bowel, and sexual function and clearly define the role of physical therapists in managing these secondary symptoms. This will hopefully empower future students enrolled in this course to have more confidence in working with this patient population and graduate from UNC’s program with a greater understanding of the impact that a spinal cord injury can have on bowel, bladder, and sexual function.
Health Literacy:
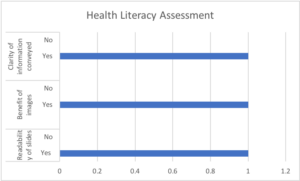
Current physical therapy students are the target audience of this capstone. Given this target audience, I created simple slides with large font and complimentary pictures to improve the readability of the presentation. The depth of information and language utilized throughout the presentation is specific to physical therapy while remaining concise and clear. Given the online, asynchronous nature of the presentation, I opted to include patient examples and periodic questions to keep listeners engaged and active throughout.9 To ensure appropriate health literacy, I included some questions regarding the clarity of information, the benefit of images, and the readability of slides into the student feedback form. Of the 22 students who completed the form, 100% indicated that these parameters were met within the presentation.
Products:
My evidence tables provide evidence-based support for the content shared and tested within my Capstone products. The tables outline the quality of life for patients with a spinal cord injury and bowel, bladder, or sexual dysfunction. They also discuss the relevant anatomy and physiology related to bowel, bladder, and sexual functioning as well as available treatment options.
Using this information, as well as information gained from the Herman & Wallace Parkinson Disease and Pelvic Rehabilitation course, I created a VoiceThread presentation. This presentation outlines the anatomy, neurophysiology, impact of injury, and treatment options for individuals following a spinal cord injury who present with bowel, bladder, and/or sexual dysfunction.
Students also received a PowerPoint copy of this presentation so they could take notes throughout the VoiceThread presentation.
Finally, I adapted the online Sakai quiz that accompanies the online study unit within the PHYT 785 course to reflect updated information expressed within my VoiceThread.
Evidence Tables:
Impact on Quality of Life Evidence Table
Anatomy and Neurophysiology of Micturition Evidence Table
Anatomy and Neurophysiology of Defecation Evidence Table
Anatomy and Neurophysiology of Sexual Functioning Evidence Table
Treatment Options Evidence Table
VoiceThread:
Quiz:
Evaluation:
My capstone advisor and committee members provided feedback throughout the development of the presentation and quiz. I also received feedback from Vicki Mercer, one of the professors of the PHYT 785 course. They provided expert advice on the content of the presentation, readability of the slides, and ways to make a virtual asynchronous lecture engaging for doctoral-level physical therapy students.
Since this project is intended for current physical therapy students, following the completion of the online study unit, I asked the UNC DPT class of ’22 to provide feedback using this form. This information was used to further enhance my presentation and improve the overall organization of the online study-unit. Additionally, I utilized the UNC DPT class of ’22’s quiz scores as another measure for my project. Overall, 90% of the class scored at or above an 80% on the quiz.
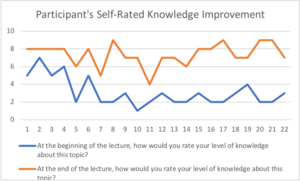
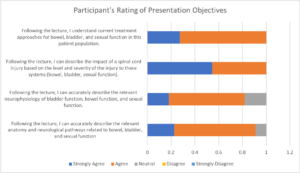
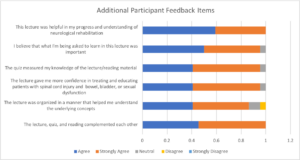
The charts provided in this section summarize the student feedback I received regarding my capstone project. Out of the UNC DPT class of ’22, 73% of them provided feedback on the survey. After the lecture, all students reported an increase in their level of knowledge about this topic. Additionally, at least 80% of students indicated that all four presentation objectives were met. Lastly, over 80% of the students found the lecture to be helpful, organized, important and improved their clinical confidence.
Self-Reflection:
I am extremely happy with the final products of my capstone project. I feel that these products seamlessly fit into the PHYT 785 course curriculum and I hope that Karen McCulloch and Vicki Mercer, the current professors of this course, can utilize my capstone for years to come. I also believe this topic will benefit future doctoral physical therapy students in their academic and professional journeys. Given the substantial impact that bowel, bladder, and sexual functioning can have on an individual’s autonomy and sense of self, I am proud that this capstone can assist in improving the knowledge gap that many providers experience when addressing these topics clinically.
Given the typical course curriculum of PHYT 785, I had to work on an accelerated timeline to ensure that my capstone aligned well within the course schedule. It was also important to receive student feedback as these products are intended for doctoral-level physical therapy students. Their feedback was instrumental in ensuring that my products were useful to their education and took into consideration their preferred learning styles. Although difficult at times, I am especially proud that I was able to submit all the necessary products in time to receive timely feedback from the UNC DPT Class of ’22 enrolled in the PHYT 785 course.
Lastly, I have a newfound appreciation for asynchronous instruction and the utilization of online teaching platforms. I experienced first-hand how difficult it is to create an engaging VoiceThread that is clear and concise. My presentation went through several iterations based on professional and student feedback regarding the clarity of the concepts. I am grateful for the experience and am proud of what I was able to accomplish.
Acknowledgments:
To Dr. Karen McCulloch PT, PhD, FAPTA, thank you for graciously agreeing to support me throughout this project. You entrusted me to adapt a portion of your course curriculum and I am so appreciative of that trust. I am grateful for your continuous support and patience throughout this process as my project underwent several iterations.
To Raheleh Tschoepe, MS, OTR/L, thank you for your expertise and gracious giving of your time and resource materials. I remember conversing with you before the inception of this project and I knew that you would be an amazing resource to have on my committee. Our preliminary conversations and project feedback really helped shape my presentation.
To Dr. Jennifer Harrington PT, DPT, WCS, CLT, thank you for providing your expertise and timely feedback throughout my capstone. Your expertise in and advocacy for women’s health and pelvic floor physical therapy allowed me to shape my presentation to educate students on treatment options available to this patient population.
To Dr. Vicki Mercer PT, DPT, PhD, thank you for entrusting me to adapt a portion of your course curriculum. I appreciated your feedback in this process as it allowed me to clarify confusing concepts within my presentation and adjust accordingly. These adjustments help ensure that future classes experience the best version of my capstone that will enhance their overall understanding of these topics.
To the UNC DPT Class of ’22, it is never easy to be the first group to experience a lecture or new teaching material. Thank you for your willingness and patience in this process as I adjusted my capstone to meet your needs as learners. Your sincere and honest feedback was pivotal to the success of this project.
Finally, thank you to my friends, family, partner, and the UNC DPT Class of ’21! These past three years have been filled with personal and professional growth and I am grateful to have had each of you play a role in this journey. For the DPT Class of ’21 specifically, I look forward to calling you my colleagues soon and can’t wait to see where your careers take you!
Sources:
- McColl MA, Aiken A, McColl A, Sakakibara B, Smith K. Primary care of people with spinal cord injury: scoping review. Can Fam Physician. 2012;58(11):1207-1216, e626.
- Guilcher SJT, Craven BC, Lemieux-Charles L, Casciaro T, McColl MA, Jaglal SB. Secondary health conditions and spinal cord injury: an uphill battle in the journey of care. Disabil Rehabil. 2013;35(11):894-906. doi:10.3109/09638288.2012.721048
- Engkasan JP, Ng CJ, Low WY. Who decides? A qualitative study on the decisional roles of patients, their caregivers and doctors on the method of bladder drainage after spinal cord injury. Spinal Cord. 2015;53(2):130-134. doi:10.1038/sc.2014.199
- Physiology and Management of Bladder and Bowel Continence following Spinal Cord Injury | Wounds Research. https://www.woundsresearch.com/article/8160. Accessed February 23, 2021.
- Hubscher CH, Herrity AN, Williams CS, et al. Improvements in bladder, bowel and sexual outcomes following task-specific locomotor training in human spinal cord injury. PLoS One. 2018;13(1):e0190998. doi:10.1371/journal.pone.0190998
- Vásquez N, Knight SL, Susser J, Gall A, Ellaway PH, Craggs MD. Pelvic floor muscle training in spinal cord injury and its impact on neurogenic detrusor over-activity and incontinence. Spinal Cord. 2015;53(12):887-889. doi:10.1038/sc.2015.121
- Deng Y, Dong Y, Liu Y, et al. A systematic review of clinical studies on electrical stimulation therapy for patients with neurogenic bowel dysfunction after spinal cord injury. Medicine. 2018;97(41):e12778. doi:10.1097/MD.0000000000012778
- Elmelund M, Biering-Sørensen F, Due U, Klarskov N. The effect of pelvic floor muscle training and intravaginal electrical stimulation on urinary incontinence in women with incomplete spinal cord injury: an investigator-blinded parallel randomized clinical trial. Int Urogynecol J. 2018;29(11):1597-1606. doi:10.1007/s00192-018-3630-6
- Plack M. Systematic Effective Instruction: Keys to Designing Effective Presentations . In: SLACK Incorporated, ed. Teaching and Learning in Physical Therapy From Classroom to Clinic. ; 2011:66-96.
Top image: https://www.backuptrust.org.uk/news/research/female-experiences-with-sexuality-after-spinal-cord-injury


11 Responses to “Understanding Bowel, Bladder and Sexual Function in a Neurologic Population: The Role of the Physical Therapist”
Debbie Thorpe
HI Sarah
Wow!!! You really produced a very complete project! Five evidence tables and a very professional, evidence-based voice thread! I know KMac is excited to be able to use this within the neuro curriculum. Your statement of need was well written and impelling. I was also impressed with how you presented your health literacy results and the results of participants’ ratings of your presentation and of participants’ learning following viewing of your presentation. You should be very proud of your products and for adhering to an accelerated timeline and still being able to get peer feedback in time to post your project! Good luck on the remainder of your clinical rotations.
Best
Debbie
Hannah Zimmer
Sarah,
Congratulations on an excellent capstone project! I am proud of you for all the hard work you have done to develop these materials, especially given the advanced timeline required of this particular project. Your voicethread, slides, and evidence tables are clear, concise, and easy to follow. I learned a lot from following along, and definitely plan to refer back to these in my future clinical practice! I especially appreciated your examples of goals for functional mobility and self care tasks–creating meaningful goals is an area where I can continue to improve, so it was helpful to consider these topics. You’ve done an excellent job with this project, and I am looking forward to seeing and hearing of your success in your residency and career in the future!
-Hannah
Sarah Richardson
Hannah,
Thank you so much! When making the Voicethread I wanted to be intentional about creating an online lecture that was informative but also engaging. I also wanted to provide concrete examples so students would be able to clearly apply this knowledge in the clinic. I am so happy to hear that you found the lecture to be helpful in your own learning. I have loved being your classmate and look forward to seeing all the great things that you accomplish as a physical therapist.
Cheers,
Sarah R.
Krista
Hi Sarah, I am so impressed with your ambition and dedication to restructuring UNC DPT’s bowel, bladder and sexual function following SCI education. The format of VoiceThread is more engaging and memorable compared to solely reading materials. I am about to start an inpatient rehabilitation rotation, so this was a perfect time for me to refresh on this topic. You did an excellent job applying principles of health literacy, which is still crucial in higher educated populations. I appreciated your concise and simple definitions throughout the presentation. I already have the VoiceThread saved to my computer for future reference. Thank you for sharing the information with me and future UNC DPTers! I am excited to see you excel after graduation and in the specialty of Women’s health and pelvic floor therapy.
Sarah Richardson
Krista,
Thank you so much! I loved being able to use this capstone to share my passion for women’s health and pelvic floor physical therapy with UNC’s DPT program. I sincerely hope you will be able to use the Voicethread for your upcoming rotation and in your professional career. I have loved having you as a classmate and look forward to seeing all the amazing things you do as a physical therapist in the future.
Cheers,
Sarah R.
Brandon Surber
Hey Sarah! This project looks so cool and I am happy to know you completed a project in an area that I know you are so passionate about (it always radiates from you when you speak on pelvic floor PT, which is something that is always great to see from individuals with dedicated interests). It seems like a daunting project to take over an entire unit of a course, but you did it extremely well. Your evidence tables are detailed and provide a great overview of the literature within the subsections of your project and the VoiceThread will be an excellent resource for students to have in the future of the neuro course. While I am not currently planning to pursue a career in the neuro specific population/setting, I am happy to know I have access to these wonderful resources in the future if needed! Also, of we end up working in the same area, I know who my pelvic floor and women’s health referrals are going to! Hope you are doing well!
Best,
Brandon
Sarah Richardson
Brandon,
Thank you so much for your kind words! Because I was able to explore my passion for this capstone, it made the work feel less daunting. I have loved learning from you as a classmate and wish you all the best in your future career. I know you will do great things!
Cheers,
Sarah R.
Karen McCulloch
Excellent job on this project, Sarah – you really took this on and did such a good job in improving the unit that students have exposure to – I’m sure that your work will pay dividends with students for years to come. I’m happy that you put the effort into it…I know you’re going to do great things with your focus on pelvic health. Thanks for helping us improve our course!!!
kmac
Sarah Richardson
Kmac –
Thank you so much for your kind words and for trusting me with this project. I truly appreciated the opportunity to share my passion within your course curriculum. I hope this small contribution to your course helps future students provide excellent care and feel a bit more comfortable when working with this patient population. I certainly have a greater appreciation for teaching after this experience. Thank you for all the work you do for the UNC DPT Program and the PT profession.
Cheers,
Sarah R.
Brianna Colello
Sarah,
Congratulations on an amazing and impactful capstone project! Its wonderful to see you pursue your passion for pelvic health PT. I am grateful for this topic and presentation as I hope to work with a large neurologic patient population in my future career. Your Voicethread and resources are very informative and I believe they can also relate to many other neuro patient populations! I especially appreciate how you include sexual function and the role of PT. I’m grateful to have you and these products as resources for my future career. Thank you for sharing your passion for pelvic health with us, I am excited to see you succeed in your future career!
Best,
Bri
Sarah Richardson
Bri –
Thank you so much for your kind words. I loved being able to share my passion through this capstone project with you all and UNC DPT. I do hope this Voicethread can serve as a future reference for you in your career. I hope it also helps future students within the UNC DPT program understand these topics and feel more confident providing patient education or referring these patients to providers who can round out a patient’s health care team.
Cheers,
Sarah R.