Neonatal Cranial Molding and Positioning Changes Related to Respiratory Device
Ashley Hite, SPT
Background
When I began pursuing my Doctorate of Physical Therapy at UNC-Chapel Hill, I knew I enjoyed various aspects of working with the pediatric population. I knew I loved the innocence, individuality, and innovation that children bring into the clinic. Thanks to my background in athletics and coaching, I also enjoy and value working with the entire family unit and how the scope of pediatric physical therapy services extend further than the time spent in the hospital or clinic. As didactic education began, I fell in love with learning and exploring human development of all forms. I found motor, neurological, and genetic development fascinating and worked to further explore these concepts. All these interests and desires were finally affirmed once I began hands-on work with children in the clinic. I love the holistic environment pediatric physical therapy fosters. Children and their environments are constantly changing and progressing, pushing us as physical therapists to continue to grow and learn as well. I also love how pediatrics presents the opportunity to work with a variety of specialties. In one day you can see patients with neurological, genetic, orthopedic, pelvic health, oncological, and many other conditions. Pediatrics always keeps you on your toes, allows you to form special relationships with both parents and families, and constantly presents the opportunity for growth as a therapist.
While on my second clinical rotation, I was fortunate to have the opportunity to work in the neonatal intensive care unit (NICU). While my time was limited due to the COVID-19 pandemic, I was immediately captivated by the NICU environment and the unique role physical therapists serve. It is an incredible and humbling experience to be able to help support these precious young lives and to be able to walk through this stressful time with caregivers and families. I love the relationship, education, and support therapists are able to provide throughout these difficult situations. When I learned of the opportunity to work with Dana McCarty in this specialty area I immediately knew I wished to pursue this incredible opportunity. Throughout my experience in the program, I have been extremely fortunate to work with mentors that lead and help progress the field of physical therapy in both practice and research. I aspire to be knowledgeable and experienced in a variety of clinical settings, but ultimately wish to pursue a career in pediatrics. I hope to be an advocate, resource, and promoter for the families and communities I am a part of.
Statement of Need and Purpose
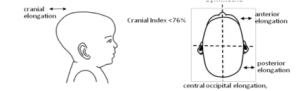
Every year, over half a million babies are born preterm in the United States with many of these infants requiring prolonged NICU stays1. While in the NICU, infants may be subjected to many different devices, like those providing supplemental oxygen, and may spend extended periods of time in certain positions. Medical devices and prolonged positioning can lead to alterations in cranial molding and infant head shape2. There are many different forms of cranial molding that can develop based upon certain areas of the infant skull that are receiving increased pressure, for example: deformational dolichocephaly. Deformational dolichocephaly is characterized by a long, slender head shape that typically results from extreme head rotation to one side or through increased usage of respiratory devices3.
Abnormal cranial molding is a complex, multifaceted deformation commonly seen in premature infants. Premature infants in the NICU, especially those of very low birth rate, are at increased risk for developing head and cranial molding deformities due to increased malleability of the neonate skull, weight of gravity, and their often sustained supine positioning2,3,4,5. Furthermore, cranial molding abnormalities have been linked to adverse motor outcomes, which are believed to contribute to early motor delays, asymmetrical motor performance, and result in an increased need for outpatient physical therapy services2. It is hypothesized that for successful treatment of dolichocephaly, systematic positional changes are needed to overcome the mechanical forces repetitive positioning places on head shaping of preterm and/or very low birth weight infants4-7.
Premature infants are also more susceptible to acute respiratory distress and mechanical ventilation to stabilize ventilation and oxygenation2,3. During this time continuous positive airway pressure (CPAP) machines are used to provide continuous airflow and stabilize blood gas levels in preterm infants3. These machines can apply pressures to certain areas of the cranium, resulting in abnormal cranial molding and poor head growth3,4. During this time positioning is commonly used by pediatric physical therapists as an intervention strategy to promote normal development and help with oxygenation; however, increased time spent in any one position can cause deformational pressures to the cranium, possibly resulting in abnormal cranial molding2-4. Literature indicates that multiple factors impact oxygenation status and cranial formation in preterm infants. The purpose of this study was to examine the interplay of these factors and their effects on cranial molding, particularly the development of dolichocephaly.
Overview
Positioning is a common intervention to improve oxygenation and respiration in patients of all ages. In preterm infants the use of CPAP machines can impact the frequency of positional changes and the variations of positions available. Positioning has further implications for both respiration, motor outcomes, and normal cranial development4-6. In 2019, the UNC Neonatal Critical Care Center (NCCC) changed the type of CPAP device they utilized with patients. Due to device design, differences in patient positioning and cranial molding were hypothesized. The purpose of this capstone project was to assess the role of positioning and CPAP device type on infant cranial molding.
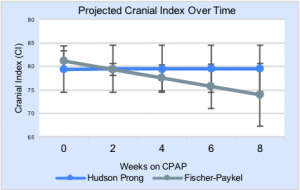
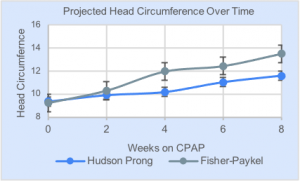
Twenty preterm infants (less than 32 weeks’ gestation) in the NCCC requiring CPAP were included in the study. Ten infants used the Hudson CPAP and ten used the Fisher Paykel CPAP. Cranial index (CI), a measure of head narrowing (assessing presence of dolichocephaly), and head circumference (HC) were obtained weekly by trained physical therapists. Infant positioning (supine, sidelying, and prone) were also retrospectively reviewed in the medical chart. Furthermore, covariates including birth weight, gestational age, days on CPAP, and hospital length of stay were collected throughout the study. Results indicated that projections for the Fisher Paykel CPAP device indicate a larger HC over time compared to the Hudson CPAP, and that the Fisher Paykel use contributes to narrow head shape with posterior occipital shift. Hudson CPAP projections suggest a slower rate of HC change over time and contribute to a superior shift of the cranial bones and flattening of the occiput. This allows HC to stay relatively stable based on the bony measurement landmarks utilized. Our study demonstrates that CPAP devices have differing impacts on CI and HC. We hypothesize that CPAP devices impact the variety of positions used and may impact the long term motor development, but further research is still needed.
Products
With Dana McCarty, I created a poster presentation to outline the findings and results of the research project. We are presenting at an upcoming research conference at UNC-Chapel Hill and have discussed presenting at a variety of other conferences throughout the year.
Evidence table describing the parameters and findings of relevant literature and further research studies.
Literature review discussing current knowledge around infant positioning, cranial molding, and the role of oxygenation status.
Evaluation
Feedback was given and incorporated throughout my capstone project from both my advisor and committee members. A final evaluation form for the poster presentation was created in order to receive formal feedback from peers, physical therapists, and other health care professionals. Feedback was collected on the quality of products, ease of understanding, and usefulness of graphs and pictures.
Link to evaluation form: here.
Self-Assessment
I am extremely thankful to have had the opportunity to complete research in the neonatal intensive care unit while working with and learning from Dr. McCarty and many other health professionals. I believe I have learned and grown immensely from this project, both academically and personally. This project taught me how to thoroughly review the current literature, dissect for correlations and connections, and combine ideas and perspectives to help answer clinical questions. Furthermore, this project challenged me to analyze data, helping further develop my understanding of statistics and how to develop products and graphs from the data. I also believe the project will help me be a better clinician as it has greatly increased my appreciation for evidence-based practice and always being able to provide your patients with the most up-to-date and highest quality of care available. I am proud of the work that has come out of this project, and I am extremely excited to have the opportunity to continue to share our findings with others. I hope to be able to take this knowledge and experience into my career, striving each day to become a better clinician and professional.
Acknowledgements
I would first like to thank my advisor and mentor, Dana McCarty. I greatly appreciate all of your help, support, and guidance throughout this project. Thank you for your constant encouragement, dedication, and countless hours spent working with and helping me through the various aspects of this project. Also, thank you for your mentorship, example, and leadership in the field of pediatrics.
Kerry Blazek and Mae Thomas: Thank you both so much for being a part of my capstone committee. I know you both are extremely busy, and I greatly appreciate you taking the time to help assist and support me throughout this project.
Debbie Thorpe: Thank you for guiding us all throughout the capstone project and always answering the endless questions I am sure we all had. Your dedication and support is greatly appreciated.
Classmates and Faculty: I just want to say a big thank you to everyone for their encouragement and support throughout the past three years. So many patient lives are going to be greatly impacted and I cannot wait to see all of the incredible things everyone is able to do. I was also able to work on this project with Anna Brown, and I just want to say thank you for your support and partnership throughout this project. It was a great learning experience and gave me someone to bounce ideas off of and problem-solve with. Also, to our incredible faculty, thank you for your endless support. I feel so fortunate to have had the opportunity to learn from each of you and greatly appreciate the time and effort put into helping us grow and succeed, as both professionals and individuals. Thank you to everyone!
References
- Preterm Birth | Maternal and Infant Health | Reproductive Health | CDC. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm. Accessed April 9, 2021.
- Crofton PM, Shrivastava A, Wade JC, et al. Bone and collagen markers in preterm infants: relationship with growth and bone mineral content over the first 10 weeks of life. Pediatr Res. 1999;46(5):581-587. doi:10.1203/00006450-199911000-00015
- Sweeney JK, Gutierrez T. Musculoskeletal implications of preterm infant positioning in the NICU. J Perinat Neonatal Nurs. 2002;16(1):58-70. doi:10.1097/00005237-200206000-00007
- Ifflaender S, Rüdiger M, Konstantelos D, Wahls K, Burkhardt W. Prevalence of head deformities in preterm infants at term equivalent age. Early Hum Dev. 2013;89(12):1041-1047. doi:10.1016/j.earlhumdev.2013.08.011
- Madlinger-Lewis L, Reynolds L, Zarem C, Crapnell T, Inder T, Pineda R. The effects of alternative positioning on preterm infants in the neonatal intensive care unit: a randomized clinical trial. Res Dev Disabil. 2014;35(2):490-497. doi:10.1016/j.ridd.2013.11.019
- Brunherotti MA, Martinez EZ, Martinez FE. Effect of body position on preterm newborns receiving continuous positive airway pressure. Acta Paediatr. 2014;103(3):e101-5. doi:10.1111/apa.12504
- Hough JL, Johnston L, Brauer SG, Woodgate PG, Pham TMT, Schibler A. Effect of body position on ventilation distribution in preterm infants on continuous positive airway pressure. Pediatr Crit Care Med. 2012;13(4):446-451. doi:10.1097/PCC.0b013e31822f18d9



4 Responses to “Neonatal Cranial Molding and Positioning Changes Related to Respiratory Device”
Dana B McCarty
Ashley – what a great job on this project! I am so pleased with how you and Anna presented this data and I am looking forward to moving ahead with a manuscript to publish. Your poster is clean, well-organized, and easy to follow. Congratulations on a job well done! I also enjoyed reading your background statement…yay peds!
Dana
Debbie Thorpe
Ashley
Well done project. I enjoyed reading your background and statement of need sections. Very complete literature review and professionally done poster. I learned some new information! The graphs in your overview are very informative and add to understanding of conclusions. Good luck on poster presentations! Have a great experience on the rest of your clinical rotations!
Best
Debbie
Ana-Clara Caldwell
Ashley, I thoroughly enjoyed reading through your project and learning about the effects of the CPAP machine on cranial molding! You have been my fellow peds partner throughout the program, and I am proud of you and the work you have done on this project! I spent the day in the NICU working with the therapists and they were explaining to me the impacts that positioning and handling have on cranial molding. However, they did not mention the impact that the CPAP has! I found it interesting that different CPAPs impacted cranial molding differently and was intrigued by your discussion as to why they result in such differences. Your poster presentation is easy to understand and gives a great overview of the study and results! I hope to see it at a conference some day! I know that this is only the beginning of great research and discoveries that you will make throughout your career, and I am grateful to have learned something new to carry with me into clinic!
Best of luck,
AC
Katie Solheim
Hey Ashley!
I was really excited to read about your capstone project due to my similar love for pediatrics and fascination with the NICU environment. On my current clinical rotation, I have had the opportunity to visit the NICU twice now with my CI. While I haven’t been able provide extensive positioning recommendations, a large part of my CI’s job (PT in the OP pediatric clinic attached to the hospital) is to work as part of a multidisciplinary team to perform 6 month, 12 month, 18 month, and 2 year follow up evaluations for infants who spent time in the NICU. I have witnessed the effects a prolonged NICU stay can have on infant head shape, but I had no idea the implications cranial molding abnormalities could have motor outcomes. After reading about your capstone project and viewing your poster I am even more intrigued to find out the type of CPAP device utilized with patients at Cape Fear Valley Hospital. Your evidence table is extremely comprehensive, and I look forward to following research on this topic!
Best, Katie