Manual Facilitation Techniques for Common Gait Impairments Post Stroke
Natalie Stein, SPT
Background:
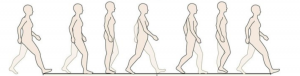
Stroke is the fifth leading cause of death in the United States and is one of the principle causes of disabilities in all industrialized countries. 1,2 In fact, almost 60% of individuals still exhibit motor impairments following standard stroke rehabilitation.1 One of the largest motor impairments that impacts disability following stroke is reduced gait performance.1 Common gait impairments include decreased gait speed, decreased endurance, reduced weight-bearing on the paretic limb, decreased stance time on the paretic limb, lower limb asymmetry, and limited range of motion, to name a few.1,3,4 Regardless of setting, a physical therapist will undoubtedly work with patients who have suffered a stroke at some point in their career, whether they are treating them immediately post stroke or observing prevailing disabilities years following a stroke. It is therefore important that all therapists are aware of how to work with these patients and are knowledgeable of different gait training interventions.
Project Interest and Statement of Need:
This project originally came to my mind during my third clinical rotation at an outpatient neuro facility. During this clinical we worked with many patients who had suffered a stroke. Along with being one of the most prevalent disabilities, impaired gait was also one of the most difficult and frustrating impairments I worked with because of my lack of intervention ideas. I knew from my neuro class that functional activity was the key to recovery, but I struggled with finding “functional” activities for rehabbing gait other than purely walking with the patient. This was something that the patient could most likely work on at home and I found it difficult to justify billing a patient for my lack of “skilled” intervention.
Luckily, during this rotation my CI taught me some valuable manual facilitation techniques that I was able to use while working on a patient’s gait. These techniques required hands on assistance and facilitation from the therapist in order to make necessary adjustments to improve gait. I observed how well these patients responded to manual facilitation both subjectively and objectively.
When I came back from that third clinical I spoke with other students who had a neuro experience as well. These students also agreed that they felt as if they had a lack of intervention ideas when it came to working on gait with patients post-stroke. These conversations sparked my interest in creating a capstone project that demonstrated the manual facilitation techniques I had learned that summer for the future second year students about to begin their neuro clinicals.
Guiding Research:
Unfortunately, the literature and research for manual facilitation is extremely scarce. Most of the research on gait rehab is focused on treadmill training, body weight support training, orthoses, and various electric modalities. However with much reading, research, and guidance from my committee I was able to piece together different literature that helped support and guide my project.
The three intervention approaches I found that most strongly correlated to manual facilitation were Proprioceptive Neuromuscular Facilitation (PNF), Neuro-Development Treatment (NDT), and the Motor Learning approach developed by Carr and Shepherd.1–3 PNF and NDT both focus on the use of therapeutic handling by the therapist in order to facilitate correct movement patterns. These approaches place emphasis on providing sensory feedback via manual contacts with the goal of increasing the patient’s awareness to areas of muscle weakness, poor activation, or poor proprioception. 2–7 The Carr and Shepherd approach emphasizes the brain’s plasticity and its ability to recover following a lesion if appropriate feedback is presented.1 This approach is less focused on manual facilitation; however, it does stress the importance of enhanced sensory feedback from the specific body part and the need to perform specific and functional movement during rehab. 1These three theories, along with an understanding of the basic gait impairments following stroke, helped guide my project.
Project Overview:
My Capstone Project is designed to be a supplemental presentation for second year students in the stroke section of PHYT 784 (Neuromuscular Intervention 1). I spent the first half of the semester completing the research previously described and speaking to different clinicians about their use of manual facilitation in the clinic. I then created videos demonstrating common gait impairments following stroke as well as the manual facilitation techniques to correct them. My final project is an easily accessible presentation that includes an overview of manual facilitation, a description of the common gait impairments seen post stroke, and the videos I created to teach students how to perform this intervention.
Project Presentation:
Manual Facilitation Techniques for Common Gait Impairments Post Stroke
Evaluation
Since I will be graduating prior to the fall semester when PHYT 784 is held, I am unable to present my project to the second year class as I had originally desired. In order to gather feedback about my presentation I therefore asked students who had previously taken this course to evaluate my presentation and its potential value to future students in the form of an online survey. I also asked for feedback from my committee members and capstone advisor. I received valuable feedback from all participating parties and was able to make necessary changes prior to submitting the final product. The survey I sent students is linked below.
Self Reflection
Overall, I am very pleased with my final presentation and the work I put into it over the course of the semester. I was very passionate about creating this project because I knew it was something the second year class could benefit from, but I was also very intimidated by the lack of research. Countless times I considered changing my topic due to this. Luckily, my amazing and supportive advisor, Dr. Prudence Plummer, encouraged me to keep my original plan because she too believed my project would be beneficial.
The research I put into this project gave me a deeper understanding into the various approaches used in neurological rehabilitation. Even if the approaches I studied had nothing to do with manual facilitation, I still found them beneficial to other areas of practice. This project also allowed me to use the knowledge and skills that I’ve acquired throughout school in order to clinically reason, evaluate, and treat disabilities despite lack of literature.
In conclusion, I believe that the presentation will be a valuable tool for students in PHYT 784 and especially valuable prior to students about to begin a neuro clinical.
Acknowledgements:
First and foremost, I must thank my incredible advisor Dr. Prudence Plummer, PT, PhD. I have no doubt that I would have been unable to complete this project without her. She not only answered my incessant emails immediately, but also taught me some of the very skills I present in my project. Dr. Plummer gave me the confidence to complete this project despite my weariness of available research and was able to meet with me almost every week during my routine panic attacks over the project.
I am also very grateful to my committee members Dr. Vicki Mercer, PT, PhD and Kara Jarboe, PT. Dr. Mercer, one of the professors for PHYT 784, allowed me the opportunity to create this project for her class and Kara Jarboe, my CI during my outpatient neuro clinical, is the person who originally taught me about manual facilitation techniques. Both of these individuals gave me valuable feedback throughout the capstone process and helped make my project what is it today.
Of course, I could not forget my wonderful two classmates who helped me film the videos for this project, Carly Bernadotte and Hailey Guerin. Thank you so much for taking the time out of your crazy schedules to travel with me to Hillsborough and assist in these videos.
Finally, thank you to all of my classmates who evaluated this project in such a timely manner and to University Physical Therapy in Hillsborough for allowing me to film in your clinic.
References:
- Belda-Lois J-M, Mena-del Horno S, Bermejo-Bosch I, et al. Rehabilitation of gait after stroke: a review towards a top-down approach. J Neuroeng Rehabil 2011;8:66. doi:10.1186/1743-0003-8-66.
- Understand Stroke | Stroke.org. Available at: http://www.stroke.org/understand-stroke. Accessed April 19, 2018.
- O’Sullivan SB, Schmitz TJ, Fulk GD. Physical Rehabilitation. 6th ed. Philadelphia: F.A. Davis Co.
- Carr JH, Shepherd RB. Neurological Rehabilitation: Optimizing Motor Performance. Oxford: Butterworth-Heinemann
- Bogey R, Hornby GT. Gait training strategies utilized in poststroke rehabilitation: are we really making a difference? Top Stroke Rehabil 2007;14(6):1-8. doi:10.1310/tsr1406-1.
- Adler SS, Beckers D, Buck M. PNF in Practice: An Illustrated Guide. 3rd ed. Heidelberg: Springer
- Eng JJ, Tang P-F. Gait training strategies to optimize walking ability in people with stroke: a synthesis of the evidence. Expert Rev Neurother 2007;7(10):1417-1436. doi:10.1586/14737175.7.10.1417.
- NDTATM: Neuro-Developmental Treatment Association. Available at: http://www.ndta.org/whatisndt.php. Accessed March 27, 2018.
image source: https://musculoskeletalkey.com/fundamentals-of-human-gait/

5 Responses to “Manual Facilitation Techniques for Common Gait Impairments Post Stroke”
Carla Hill
Natalie,
Very good work on your Capstone! I applaud your effort to stick with the project despite a lack of direct evidence. In clinic practice, there are many gaps that aren’t clearly answered in the literature, so we draw on related theories and apply clinical reasoning as you did here. The video is a helpful education tool for future students to be introduced to facilitation techniques they can practice on each other and apply in the clinic.
Carla
Martha Kalisz
Hi Natalie,
I enjoyed listening to and learning from your voice thread presentation, and appreciated the well organized and clinically relevant information that you were able to provide. I have not personally worked with a population of patients with stroke in an outpatient setting, and so I haven’t experienced using these techniques in practice. However, I can definitely relate to your in-clinic learning of manual facilitation techniques. In my clinical experience in the pediatric setting, my clinical instructor also taught me multiple manual facilitation techniques that I hadn’t been aware of prior to clinical experiences. Using manual facilitation with pediatric patients to effect impaired gait seemed to be helpful, as well! However, I was not as astute as you were to ask the deeper questions as to why these techniques were working and what we as therapists were affecting. I will definitely use your materials as a resource if I find myself working with stroke patients, and will also see if I can find if similar techniques are used with pediatrics! As far as I know, there is very little research for using manual techniques in the pediatric population as well, but I liked your rationalization for looking at research from theories using similar principles such as PNF or NDT as guiding principles. Great job gathering clinically relevant information on a tricky subject! And thank you for an excellent resource.
Andrea Stewart
Natalie, I really enjoyed learning about your experiences designing a project that lacked strong evidence. I can imagine that designing a study to evaluate manual facilitation for gait impairments is tricky due to the difficulty of trying to quantify manual facilitation. I am so impressed with your perseverance and ability to apply theories from PNF, Carr and Shepard, and NDT. I found your presentation very valuable. I would have loved to have had access to this prior to my outpatient neuro rotation. Hopefully, it will be integrated into future courses and the facilitation techniques you cover will make their way into hands-on labs in our program. Excellent job!
Prue Plummer
Natalie, I love how this turned out! You really did a great job to develop this resource for your peers, and it is going to be tremendously valuable. I know how much work you put into this, and how deterring it can be when you can’t find any evidence. You persisted in spite of these challenges, and I can tell how much you learned. I’m very proud of you!
Thank you for the very kind acknowledgement. It was my pleasure to help and guide you on this.
Wishing you ongoing success in your career.
Prue
Greg Howell
Natalie,
As a fellow student who utilized/learned a myriad of manual facilitation techniques during my inpatient rehabilitation clinical experience last spring, I was really happy to see this topic addressed. While we certainly were exposed to similar and related techniques in class, none were directly applied to the help facilitate gait, during gait (from what I can remember), so the information you’ve presented is definitely useful in that regard. I feel that your presentation is designed well, flows nicely, and is easy to follow as it moves from one gait deviation/facilitation technique to the next. Adding the ‘hand placement’ and ‘facilitation techniques’ text descriptions the “notes” section of each video slide really helps to supplement the information presented in the video, and will definitely help students when it comes to remembering these techniques for practical/clinical purposes. One suggestion I have is that because these techniques require specific and timely hand placement and sequencing, practice should really be emphasized in presentation. Perhaps after each video slide, or at the culmination of the entirety of the presentation, whatever you believe is best. I just think to truly understand these techniques, one needs to not only understand them, but also experience them. Really great job with this overall, and I wish we had this last year!