The Impact of COVID-19 on Rehabilitation Practice: A Clinician Perspective
Raiya Feinberg, SPT and Heather McGovern, SPT
Background
COVID-19, also known as coronavirus, is a respiratory disease first discovered in late 2019 that has reached pandemic status since its initial discovery and has greatly impacted people and health systems across the globe.1,2 COVID-19 is spread via the transmission of respiratory droplets from an individual that has been infected by the SARS-CoV-2 virus, the viral agent that causes COVID-19.1 To further complicate the spread of coronavirus from person to person, individuals infected with the virus may present with a wide range of symptoms, from asymptomatic presentations to those facing hospitalization or even death.1 These symptoms may present anywhere from 2 – 14 days from the time of exposure and most commonly include symptoms of fever, loss of taste and or smell, shortness of breath, and cough.1,3 Case trends and research have revealed that the populations most at risk for severe cases of the coronavirus are older adults or those with underlying medical conditions.1 These more severe cases, often resulting in hospitalization, include presentations such as trouble breathing, chest pain, respiratory distress, and possible death.1,3
The World Health Organization recognized the discovery of COVID-19 in the early days of January 2020 in Wuhan, China with the first case of coronavirus reaching the United States later that month on January 21, 2020.4 In addition to cases in the United States, COVID-19 rapidly spread to countries across the globe, creating fear and the declaration of COVID-19 as a Global Health Emergency, and eventually, as a Global Pandemic on March 11th, 2020.2,4 In 2020 individuals across the world have coped with quarantines, extended shutdowns, mask mandates, social distancing, fear of exposure, worry for loved one’s safety, personal protective equipment shortages – to name just a few of the challenges faced. Since coronavirus’s arrival to the United States over 20 million cases have been reported across the country, resulting in over 346,000 deaths.4 Due to the novelty of this virus and its impacts on both the individual person and society as a whole, there is a need for current and future research. As 3rd year Doctor of Physical Therapy students, we joined Dr. Jessica Cassidy’s lab, the Cassidy Plasticity Lab at the University of North Carolina at Chapel Hill, to expand our understanding of the impacts of COVID-19 on the rehabilitation teams in both acute care and inpatient rehabilitation settings. Recruitment and data collection for this research study began in September 2020 and continued through November 2020. Data analysis and interpretation continued through the winter and spring of 2021, with hopes of publishing a future manuscript.
Statement of Need
As a year has passed since the outbreak of the COVID-19 global pandemic, there is certainly an opening for current and future research surrounding this disease and its impact on patients, therapists, and the healthcare system as a whole. The goal of this research project was to evaluate the impacts of COVID-19 on rehabilitation therapists (Physical Therapists, Occupational Therapists, and Speech-Language Pathologists) working within the acute care or inpatient rehabilitation settings during COVID-19. Specifically, this research aimed to collect qualitative interviews and quantitative data on depression and burnout to create a holistic picture and to write a story of the experiences of therapists while working through the pandemic. As COVID-19 is still evolving this research is timely and much needed as rehabilitation units and hospital systems as a whole evaluate and consider their response to COVID-19 in the past year and learn how to move forward and be better prepared for future challenges.
Purpose and Overview
The Impact of COVID-19 on Rehabilitation Practice: A Clinician Perspective, is a mixed-methods study, using a concurrent triangulation design with a convergence model, conducted during the COVID-19 pandemic. The primary aim of the study was to explore the experience of rehabilitation therapists working as healthcare providers during these unprecedented times via qualitative interviewing and quantitative outcome measures. Specifically, this study explored the impacts of changing policies and procedures on therapist interactions with patients, their coping mechanisms, and feelings of burnout and depression during the pandemic.
Structured qualitative interviews were conducted to create a picture of these experiences. Interview transcripts were analyzed through a process of coding, categorizing, and identifying themes. Quantitative measures, specifically the Beck Depression Inventory and the Oldenburg Burnout Inventory were utilized to assess therapists’ feelings of burnout and depression while coping with the changes in life and practice brought on by the pandemic. Participants in the study included occupational therapists, physical therapists, and speech-language pathologists working in inpatient rehabilitation or acute care settings in a large hospital system during the COVID-19 pandemic.
Based on our research, we were able to develop models to serve as visual representations of the data. We created both a PowerPoint presentation to deliver at an in-service as well as a handout explaining the models to provide to therapists at UNC Hospital via a virtual presentation session.
Products
Inservice Presentation
April 30, 2021, we will host an in-service event to present the research and findings of the study to the UNC Hospitals Rehabilitation Department. Below we have included a pdf link to the PowerPoint presentation that we will utilize to aid in delivering the presentation.
Inservice Presentation: The Impacts of COVID-19 on Rehabilitation Practice: A Clinician Perspective
Models
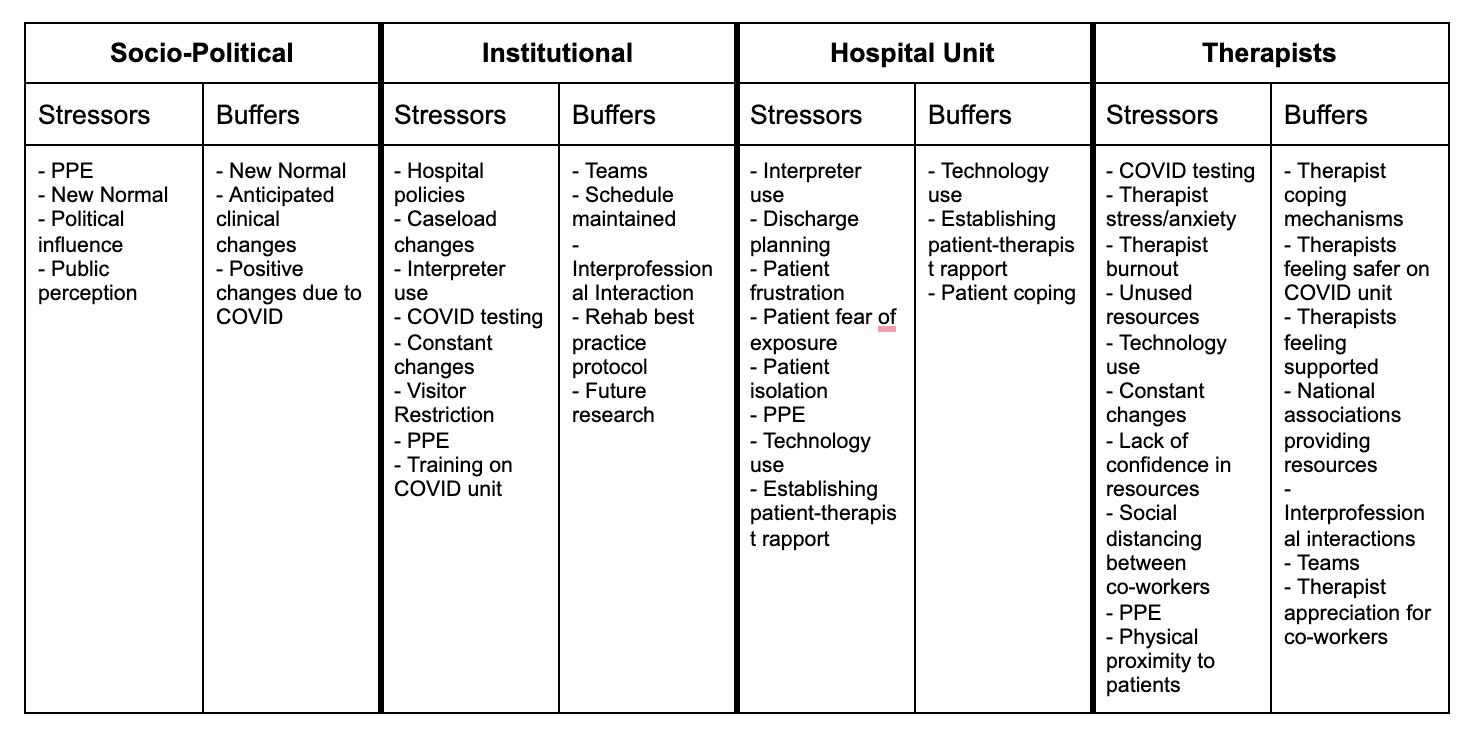
Figures 1 and 2 depict the findings from the analysis of the qualitative interviews. These figures were generated after multiple rounds of coding by several members of the research team. Coding involves combing through transcriptions of each therapist interview and creating key terms or phrases that summarize the thoughts or ideas stated by therapists. These individual codes were then grouped into broader categories and used to create key themes. This iterative process was used with the full research team to enhance the rigor and trustworthiness of the findings.
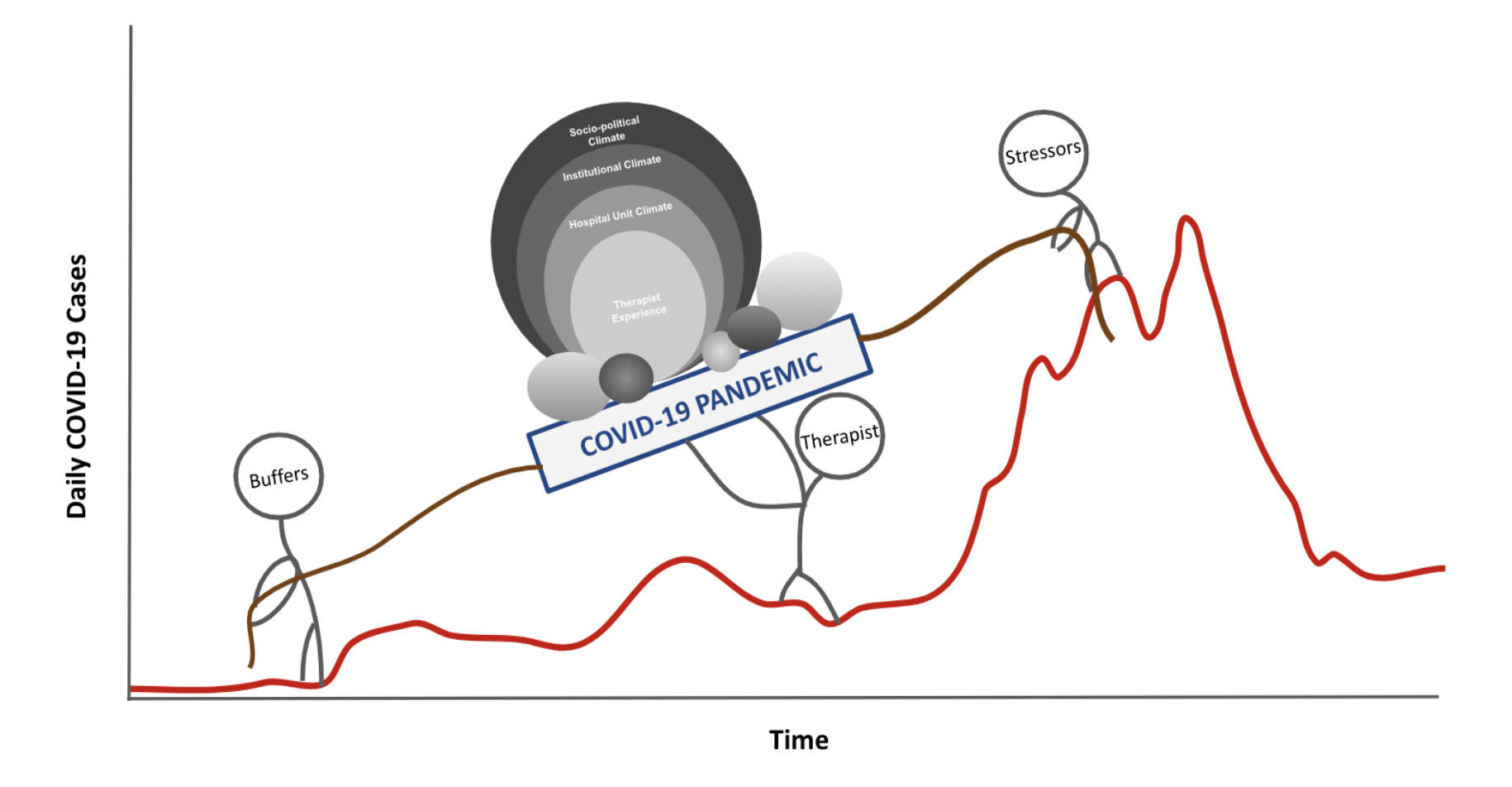
Fig. 1: Impacts of COVID-19 on Rehabilitation Practice Model
Figure 1
Figure 1 illustrates how therapists were impacted and influenced by both stressors and buffers throughout the COVID-19 pandemic. To illustrate this in a more meaningful way, daily cases of COVID-19 diagnoses are used as the ‘hill’ therapists have been climbing and overcoming as frontline healthcare workers. Our analysis revealed that while there were many stressors that therapists encountered during the COVID-19 pandemic, there were also buffers that made coping with these challenging times more manageable. For example, shortages of personal protective equipment (PPE) and the physically taxing nature of donning/doffing PPE were generally considered as stressors, while coping mechanisms such as spending time with immediate family or participating in physical activity outside of their work environment served as buffers to lessen the load and stress felt by many clinicians. The stressors and buffers influence the load that the therapists carry by pulling the therapists in a backward or forwards direction, respectively.
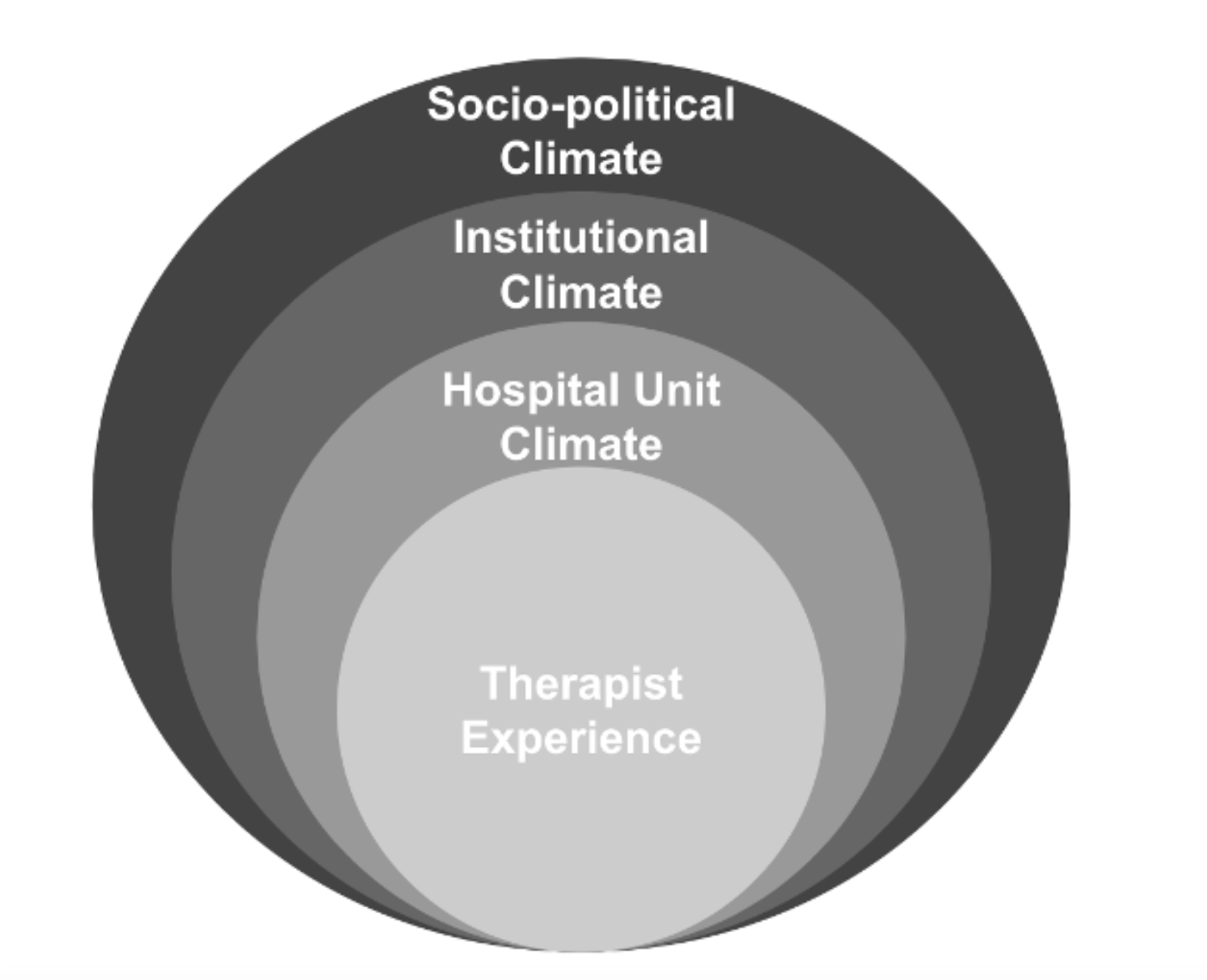
Fig. 2: Key Themes
Figure 2
Figure 2 depicts the load the therapists have dealt with and adapted to during COVID-19. This model represents the four key themes. The model is structured utilizing concentric circles to illustrate the interconnectedness of these key themes, all of which have interacted with one another during the COVID-19 pandemic. Each key theme and its underlying codes are influenced by the adjacent circles, each impacting one another in various ways. Based on qualitative data from interviews, it was found that the socio-political climate surrounding the pandemic directly influenced changes at the institutional level. These institutional policy changes led to changes in individual hospital units and therefore affected the clinician’s experience on each unit. Within each key theme, stressors and buffers were identified that influenced not only the theme itself but also how these themes affected one another. Below are examples of stressors and buffers identified within each of the four key themes. The entirety of the codes, categorized into key themes can be found in table 1.
- Socio-political stressors included stay-at-home orders, mask mandates, public fear, and miscommunication that swept the nation during the pandemic. Buffers included the newfound appreciation for healthcare workers and other essential workers, current and future strides in research that have resulted from the pandemic, as well as the development of a vaccine.
- Institutional stressors included visitor restrictions within hospitals, constant changes in hospital policy, an overall lack of COVID-19 tests, and PPE requirements and shortages. Buffers included the interprofessional relationships that have been fostered during these changes as well as the creation of a new “best practice” protocol amongst rehabilitation professionals in response to COVID-19.
- Hospital unit stressors included challenges with discharge planning, difficulties acquiring interpreter services, patient fears and frustrations, unit-dependent variations in PPE requirements, and a lack of interaction with a patient’s family/caregivers. Buffers included the use of technology to work around in-person restrictions, an increased patient/therapist rapport, and therapists’ feelings of safety on COVID units due to appropriate equipment and training.
- Therapists’ stressors such as fearfulness of the virus, lack of control, and managing family issues result in burnout, anxiety, frustration. Buffers included adopting new coping mechanisms to deal with these stressors and a heightened appreciation for coworkers.
Table 1. Key Themes and Individual Codes Identified During Semi-Structured Interviews with Therapists
Conclusion
Since the emergence of the COVID-19 pandemic, healthcare workers have dealt with constant changes, regularly adapting to “new normals” of patient care and standard practice. Some of these changes have led to increased stress on rehabilitation therapists, while others have helped to diminish the challenges of working in healthcare during a global pandemic. Despite these major changes, therapists have adopted coping mechanisms to diminish the impact of burnout and depression, demonstrating the continued resilience of these essential workers during COVID-19 and beyond.
Evaluation
Feedback from all of our Capstone advisors, as well as other members of the research team, was used as guidance in the creation of our presentation and models.
Additionally, we created an evaluation survey that will be available to the rehabilitation therapists for feedback after our in-service presentation, delivered on April 30, 2021. This evaluation is attached below. This feedback form was designed to measure the effectiveness of our presentation skills, as well as gauge feedback on the data presented.
Health Literacy
Our products were all designed with the intention of being delivered to other healthcare providers, specifically rehabilitation therapists, and have been created with this level of health care experience and common language in mind. Our presentation includes background on the COVID-19 pandemic followed by a brief introduction on the purpose of the study and a description of the methods. Next, the data is presented in the form of figures and tables, with verbal explanations being provided throughout the presentation. We aimed to present this story from a clinician’s point of view, including direct quotations into the presentation.
Reflections
Raiya’s Reflection
Prior to beginning this capstone project, I had no experience with mixed methods research. I was nervous when starting this project just based on the unfamiliarity but I was very excited to experience this method of research and learn how to appropriately conduct and analyze both qualitative and quantitative data. I knew this task would be challenging with my lack of prior experience; however, with the help of our amazing research team and advisors I was ready to take it on and grow as a researcher.
As many people experienced this last year, COVID-19 brought about some complications and setbacks. We had originally planned for this project to be from both an inpatient clinician and patient perspective; however, we were unable to reach out to and meet with enough patients to feel comfortable including their stories in the research. COVID-19 made it difficult to recruit participants and we eventually chose to not only take out the patient perspective but also widen the clinician perspective, later including both inpatient rehabilitation therapists as well as acute care therapists. When we first realized we were going to have to change paths, I was frustrated and began to worry about how we were going to present the information we had hoped. This experience taught me that there will always be complications and difficulties with research but it is important to be able to adapt. We were still able to create wonderful products that I can ultimately say Heather and I are both very proud of.
With the project taking on a new direction of solely clinicians’ stories, we moved forward with interviewing and compiling data. Through this process I was able to improve not only my interview skills but also the ability to connect with other healthcare providers going through the same pandemic. It was an incredible opportunity to be able to hear their stories and learn from their experiences. I am very excited to be able to share our findings with the therapists at UNC hospital so they are also able to learn from and grow based on the research. The knowledge I gained from each and every therapist interviewed is information I plan to take forward with me as I become a clinician.
Heather’s Reflection
After an extremely challenging year for many since the start of the COVID-19 global pandemic, I am very proud to have worked on this research project exploring the experiences of some of those most impacted by COVID-19 on a daily basis, rehabilitation therapists working in acute care and inpatient rehabilitation settings. Over the last year, I have gained a more in-depth understanding of the research process – from initial planning, recruitment, data collection, interpretation of data, and developing conclusions. With limited previous experience participating in research planning and implementation, I have gained skills across the various areas of mixed methods research that this study utilized.
One area I made significant growth in throughout this project was conducting interviews. Not only was hearing stories and opinions from all the therapists about their experiences working in healthcare throughout the COVID-19 pandemic very insightful, but it gave me the opportunity as a student to practice my interviewing skills – an invaluable skill for physical therapists throughout their career no matter the setting they may work in. Additionally, I had no previous experience with coding, the process of combing through all qualitative interview data, and creating key terms and phrases to mark important points in therapists’ responses to our interview questions. Once these codes were created one of my favorite parts of this research project was the collaborative nature of working with the other members of the Cassidy Plasticity Lab to create key themes and a conclusive model based on the study findings.
Overall, I am very proud of the work Raiya and I have put forward after many months of moving through the research process. Through each stage of this project, I have learned valuable skills in various aspects of research and fostered mentorship and learning from Dr. Cassidy, Dr. Bagatell, and other members of the Cassidy Plasticity Lab team. COVID-19 has had a significant impact on lives across the world, beginning in 2020 and likely leaving lingering impacts for many years to come, and I feel very honored to have worked on and tell the stories and experiences of these frontline healthcare workers. In the coming years, there is likely to be an abundance of literature and research studies published about this pandemic and its impacts across various disciplines as we learn and create distance from the hardest parts of the pandemic, and I greatly appreciate the opportunity to have played a role in this research.
Acknowledgments
To Dr. Jessica Cassidy, PT, DPT, PhD our capstone advisor, thank you for your guidance and mentorship throughout this research and capstone experience. Your drive, ideas, and expertise have made this project possible and we are greatly appreciative of your patience and willingness to serve as a mentor to us both. Being a part of your research lab has been an important part of our time here at UNC Chapel Hill during our third year. Your constant encouragement, advice, and leadership made this a wonderful project to work on and we are extremely grateful for the experiences with which you provided us.
To Dr. Nancy Bagatell, PhD, OTR/L, FAOTA (Associate Professor in the Division of Occupational Science and Occupational Therapy, UNC Chapel Hill), a special thank you for serving both as one of our committee members and a mentor throughout the research process. We appreciate all of the guidance and education you provided on research methods, particularly qualitative and mixed methods research from interviewing to data integration and interpretation.
To Dr. Susan Gisler, DPT, MHA (Assistant Director of Therapy Services at UNC Hospital) for serving as one of our committee members and providing us with feedback on both our presentation and products.
To Katherine Hendry and Ramis Chowdhury (Undergraduate Research Assistants, UNC Chapel Hill), thank you for being such an integral part of the research team. Your countless hours spent on interviews, transcriptions, coding, etc. made this project possible, as well as your insightful feedback and ideas as we made conclusions and models based on our data. We greatly appreciate your hard work and dedication to this project.
To Dr. Kelly Fletcher, PT, DPT, MHA (Rehab Therapy Manager, Rehabilitation Services UNC Hospitals), thank you for serving as a liaison between the research team and hospital staff and allowing us to conduct this research and share the findings.
To the Class of 2021, thank you. This year was a tough one on students everywhere, but going through it with an amazing cohort made it manageable. We are grateful for the constant support and camaraderie and cannot wait to see where all of our futures take us.
Finally, a very special thanks to all of the rehabilitation therapists who took time out of their extremely busy schedules to sit with us and share their stories during an incredibly challenging year. We greatly appreciate your honesty and vulnerability in sharing your experiences.
References
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). CDC, Disease or Condition of the Week. https://www.cdc.gov/dotw/covid-19/index.html. Published February 25, 2021. Accessed April 1, 2021.
- Johns Hopkins University & Medicine. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Johns Hopkins University & Medicine Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html. Published 2021. Accessed April 13, 2021.
- Centers for Disease Control and Prevention. Symptoms of COVID-19. CDC: COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Published February 22, 2021. Accessed April 13, 2021.
- American Journal of Managed Care Staff. A Timeline of COVID-19 Developments in 2020. American Journal of Managed Care. https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020. Published January 1, 2021. Accessed April 13, 2021.

3 Responses to “The Impact of COVID-19 on Rehabilitation Practice: A Clinician Perspective”
Vicki Mercer
Hi Heather and Raya,
Great work on this project! I love your model!! I’m sure your in-service was well-received (I hope to have an opportunity to hear about that at some point). I look forward to seeing this work published in the not-to-distant future!
Best,
Vicki
Debbie Thorpe
Heather and Raiya
Wow! What a fantastic job on this project! Very insightful results. From reading both of your self reflections, it appears that you both learned many new skills this past year (interviewing via zoom, conducting, analysis and interpretation of mixed methods research , coding qualitative interviews, …) Your in evidence-based in service on the background and results of your surveys and focus groups is very professionally presented. I think if you add a voice thread, it would enable it to be widely viewed asynchronously. I am sure your in service presentation was a huge success! This would make a great NCPTA or even CSM presentation. You should consider submitting it as an abstract. As well, a manuscript! Thank you both for this valuable work.
Best
Debbie
Jessica Cassidy
Heather,
Thank you for a wonderful Capstone reflection. It makes me very happy to hear that you enjoyed the research process and experienced personal growth especially with the participant interviews. From my perspective, your confidence and ease grew significantly after that first interview! As I expressed in my note to Raiya, your willingness to “go with the flow” and adapt to several unanticipated challenges were key in the successful completion of this study. Your color-coding and artistic talents during the construction phase of our model also helped! Thank you again for being a part of this important study.