Author: Hope Arrowood, SPT
Capstone Advisor: Dr. Jeff O’laughlin, PT, DPT, OCS, FAAOMPT
Committee Members: Dr. Lindsay Morrow, PT, DPT, CSCS, Dr. Bria Dunn, PT, DPT, OCS
Background
When entering my first clinical rotation the summer of 2021, I was rather unfamiliar with how to utilize and implement a surgical protocol into my treatment sessions. I worked with my clinical instructor to learn this skill and grew to love treating post-operative patients. After speaking with fellow classmates, I realized there was a common lack of knowledge in this area for first-year students. In the Musculoskeletal 1 class, students learn about the shoulder complex, common pathologies, and procedures, but there is limited information about post-operative rehabilitation. I wanted to supplement the curriculum to help bolster the information provided about surgical protocols, time moderated tissue healing, criteria to progress the patient, and specific intervention ideas. This project aligns well with my personal and professional goals because I am interested in working in the orthopedic setting, and I enjoy treating people who are recovering from shoulder operations. Additionally, I enjoy presenting and teaching. This format allowed me to practice these skills for future use. My hope is that students will be able to apply this information in their clinical rotations and demonstrate a better preparedness to treat post-operative patients.
Statement of Need
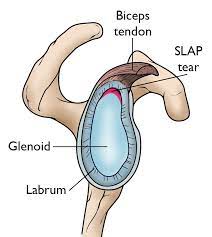
Superior labrum anterior to posterior (SLAP) lesions of the shoulder are a common pathology treated by physical therapists. This injury is most often acquired by overhead athletes, but may also be seen as a result of age related changes in the older adult population4. In my experience taking MSK-1 there was a shortage of information regarding surgical protocols and how to incorporate them into clinical practice. Approximately half of each cohort will complete a clinical rotation in an outpatient orthopedic setting shortly after the completion of the course. A basic understanding of post-operative protocols for various joints is a vital skill for students working in an orthopedic setting. Adding this information into the first-year curriculum will set UNC students up for success when completing their clinical rotations and as future clinicians.
Purpose
The purpose of this project was to build a presentation that would supplement the MSK-1 curriculum of UNC’s DPT program, provide students with introductory knowledge about post-operative treatment for SLAP tears, and to identify specific precautions and interventions for each phase of rehabilitation through the first 4 months of treatment.
Products
PowerPoint slide deck presented in person to first-years students enrolled in Musculoskeletal 1, Spring 2023.
Evaluation
Tools: Presentation Evaluation Form
The feedback I received from students was encouraging! It seems that it was a necessary and helpful topic for first-year students. The discussion about post-operative care helped connect the dots between specific pathologies and the appropriate treatment of that condition. As I expected from my own experiences, many students agreed that specific intervention ideas was the most beneficial portion to prepare for clinical work. After reviewing the feedback, I adjusted the slides to include pictures of common exercises as requested by students and my mentors. Many physical therapy interventions have unique names that are not well known by students who have yet to go on rotation. I also learned that taking time to demonstrate the exercises would have been a good lab activity to allow students to practice leading and performing the exercises. Additionally, many students mentioned that I moved really quickly through the material, which is not new feedback for me. I continuously have to remind myself to speak slowly, not rush through the information, and plan to keep practicing this skill in the future.
I led the students through an activity focusing on health literacy when speaking to patients. Not only was this was one of the students’ favorite activities, but my own as well. They worked together in small groups to brainstorm ways to explain post-operative precautions to a patient in simple, non-anatomical language that everyone can understand. Often protocols are written in medical terms, and it is extremely helpful to be able to explain complex range of motion limitation in functional and practical terms that patients can directly apply to their daily activities. That idea came from a past instructor who gave me that same assignment and I’m glad it added to the learning for this project as well!
One thing I would change in developing a future project would be allowing more time for feedback before the time to present. My presentation was scheduled fairly early in the semester and I didn’t allow adequate time for revisions before presenting. After a few rounds of feedback from my committee as I was refining the project, I saw a lot of improvement in the material and format! Overall, I learned a lot from developing this project and hope that it was helpful in developing clinical skills for first-year students.
Acknowledgements
I’d like to offer sincere thanks to Dr. Jeff O’laughlin, PT, DPT, OCS, FAAOMPT for his advice and leadership this semester! He was essential in helping narrow down a very broad project area and graciously opened up the classroom for me to present to his students. This project would not be what it is without Lindsay Morrow, PT, DPT, CSCS! Thank you for helping me with this project from its conception, and always providing the most rapid responses to my many questions! I would also like to extend my thanks to Bria Dunn, PT, DPT, OCS as a committee member for this project. Your insight into developing educational materials was a huge help, and I am very grateful for your feedback!
To my classmates in the class of 2023, thank you for your never ending support, PowerPoint troubleshooting skills, motivational high-fives, and wonderful suggestions during throughout this project and the past three years! You are some of my favorite people and I love you all!
Lastly, I’d like to mention the class of 2025, thank you for your attention and in class participation this semester! Your feedback was very helpful and I look forward to seeing you do big things in the future!
References
- Delaware Physical Therapy Clinic. Rehab Practice Guidelines for: SLAP Repair.
- Massachusetts General Hospital Orthopedics. Arthroscopic Labrum Repair of the Shoulder (SLAP).
- Brigham and Women’s Hospital Department of Rehabilitation Services. Arthroscopic Labral Repair Protocol-Type II, IV, and Complex Tears. Published online 2016.
- Christopherson ZR, Kennedy J, Roskin D, Moorman CT. Rehabilitation and return to play following superior labral anterior to posterior repair. Oper Tech Sports Med. Published online July 2017. doi:10.1053/j.otsm.2017.07.002
- Kennedy J. Rehabilitation After Upper Extremity Surgery. Lecture presented at the: PHYT 874; January 31, 2023.
- SLAP Repair Arthroscopic Double loaded anchor Y config – YouTube. Accessed April 3, 2023. https://www.youtube.com/watch?v=75ARVxXIRBE
- Killian ML, Cavinatto L, Galatz LM, Thomopoulos S. The role of mechanobiology in tendon healing. J Shoulder Elbow Surg. 2012;21(2):228-237. doi:10.1016/j.jse.2011.11.002
- Thigpen CA, Shaffer MA, Gaunt BW, Leggin BG, Williams GR, Wilcox RB. The American Society of Shoulder and Elbow Therapists’ consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(4):521-535. doi:10.1016/j.jse.2015.12.018
- Itoi E, Hatakeyama Y, Urayama M, Pradhan RL, Kido T, Sato K. Position of immobilization after dislocation of the shoulder. A cadaveric study. J Bone Joint Surg Am. 1999;81(3):385-390.
- Park MC, Idjadi JA, Elattrache NS, Tibone JE, McGarry MH, Lee TQ. The effect of dynamic external rotation comparing 2 footprint-restoring rotator cuff repair techniques. Am J Sports Med. 2008;36(5):893-900. doi:10.1177/0363546507313092

5 Responses to “SLAP Repair Post-operative Surgical Protocols and Progressive Intervention”
sarahjmc
Hope,
I’m so glad that I was able to be present for your presentation in class. I loved getting to learn from you, taking a deeper look into post-operative protocols and progressions for SLAP lesions. The shoulder is one area that I tend to have a hard time differentiating. It really helps to have memorable presentations and resources to access like the ones you have presented on and created. This is a great clinical resource, and I look forward to using this information when I get to work with a patient with this type of operation! I’m so proud of your hard work and will be asking you questions in the future!
Sarah
Jeff
It was well received in class and a nice addition to the shoulder unit for MSK 1. Well done Hope
Austin Kliewer
Hope,
I think you did an awesome job on your project and enjoyed listening to you present it to the 1st year students in MSK 1! You chose a very practical topic to focus on – one where most (if not all) of those going into outpatient orthopedics will benefit greatly from. I enjoyed how you emphasized how we might be able to educate our patients on precautions/restrictions in a way that they can understand!
rdibuono
Hi Hope,
Great job with your project! You can clearly see your passion for treating this population through your work creating the project materials. Your lecture is a great guide to treating this population and I wish I had something like this when I first learned about SLAP lesions. Everything was very thorough and well organized. My favorite aspect was your in-class activity where you had students tell each other the protocol precautions by using examples of actual activities a patient would understand. There is nothing harder than coming up with activities to match precautions on the spot while talking to patients—especially for resisted supination to limit bicep activation! Now that the first years have had this experience in a non-stressful environment, they will be able to confidently provide great examples to their patients in clinic! Again, wonderful job with this project and congratulations on wrapping up our final year!
macg
Hope,
First, congratulations on completing your capstone. It appears as though you put a lot of hard work and thought into it. I enjoyed reading over your PowerPoint presentation, it was very comprehensive and informative related to SLAP tears. The relevance of your capstone, clinically, is massive, and I find this information to be very useful moving forward into my own professional practice! I also appreciate how you included some great ideas related to interventions that coincide with the standard post-op protocol. I wish you the best of luck following graduation in your future endeavors as a new Physical Therapist!