The Effects of Metronome Frequency and Walking Environment on Gait in People with Parkinson’s Disease
By: Maddie Wygand, SPT
Background
I have a strong interest and appreciation for research and knew that I wanted to participate in a research experience while in the DPT program at UNC. I completed a research elective under the wonderful guidance of Dr. Mike Lewek, PT, PhD during the Fall 2017 semester and presented my research and results in a written manuscript and presentation at the UNC Center for Rehabilitation Care for my capstone project. I conducted this research with my classmate and co-investigator, Guneet Chawla, SPT. The inspiration for this project was fueled by our interest in the PT treatment of this patient population and our personal connections to Parkinson’s disease (PD). I had a strong desire to conduct research for PD due to my experiences with my dad who has inspired me every day since he was diagnosed with Young-Onset PD in 2004. Through our personal interests and review of the current research, we developed an idea that begins to fill a gap in the current evidence. The purpose of my research was to determine and compare the effects of metronome cueing at various frequencies on a treadmill and overground on spatiotemporal gait parameters in people with PD.
Acknowledgements
First, I would like to extend my sincere gratitude to my research and capstone advisor Dr. Mike Lewek, PT, PhD. Without his guidance, support, time, and training, this wonderful experience would not have been possible. He was just as excited about this project as I was and his enthusiasm provided encouragement throughout this entire experience. I truly appreciate the mentorship that he has provided throughout my DPT education and, especially, with this project.
Second, I would like to thank Dr. Nina Browner, MD, for her guidance throughout this entire process as well as for serving on my capstone committee. Her expertise in Parkinson’s disease provided crucial knowledge for designing this study and recruiting appropriate participants.
I would also like to thank Diane Meyer, PT, for serving on my capstone committee and providing feedback on my manuscript and presentation. She provided a valuable PT perspective for how this study and these results can impact patient care.
Finally, I would like to thank my classmate and co-investigator, Guneet Chawla, SPT, for going on this research journey with me. She brought so many unique skills and passions to this research team and I truly enjoyed working with her to make our project successful.
I am also extremely appreciative of all of the people who volunteered their time to participate in this study!
Abstract
Background: One of the most debilitating symptoms of Parkinson’s disease (PD) is the loss of motor automaticity and resulting gait abnormalities. The use of a treadmill and rhythmic auditory cues may improve spatiotemporal gait parameters in this population. Both of these techniques are often used in the treatment of PD, however, there is little consensus on how the walking environment and frequency of metronome cues change gait.
Objective: The purpose of this study is to determine the effect of metronome cues on spatiotemporal gait parameters when walking overground compared to walking on a treadmill in people with Parkinson’s Disease
Methods: Twenty-one people with PD walked overground and on a treadmill with metronome cues of 85%, 90%, 100%, and 115% of their baseline cadence. Gait speed, step length, and cadence were measured and compared for all trials.
Results: When walking overground, metronome cues of 85%, 90%, and 115% yielded changes in cadence and gait speed but not in step length. When walking on the treadmill, metronome cues of 85% and 115% yielded changes in step length while 85%, 90%, and 115% yielded changes in cadence. Gait speed did not change since the speed of the treadmill was controlled.
Conclusions: This data suggests that people with PD are able to manipulate their spatiotemporal gait parameters when provided the appropriate metronome cue and walking environment. The change in gait mechanics is dependent on the metronome cue and walking environment used. Also, the ability to accurately match the metronome cue is not as important as providing the appropriate increased or decreased frequency.
Introduction
Parkinson’s Disease (PD) is the 2nd most common neurodegenerative disorder, only behind Alzheimer’s Disease.1 The cardinal symptoms of PD include tremor, bradykinesia, rigidity, and postural instability.2 One of the most common and debilitating symptoms in PD is gait abnormalities. Common gait disturbances include decreased step length, increased variability, freezing of gait, decreased gait speed, increased double support time, and increased cadence. 3–5 These gait abnormalities are associated with decreased motor automaticity which begins to deteriorate in the early stages of PD.6 In an effort to improve gait mechanics and quality of life for individuals with PD, physical therapy is often prescribed.7 Current research has focused on various techniques that can be used for gait training to minimize the deficits.
Given the automaticity and motor deficits in PD, it is not surprising that walking on a motorized treadmill induces different gait patterns by encouraging a more automatic gait due to the continuous belt movement compared to the self-generating gait pattern overground. In particular, both individuals with PD and healthy individuals decrease gait variability when walking on a treadmill compared to overground gait.4 Unlike healthy adults, individuals with PD are known to take increased step lengths and decrease the cadence when walking on a treadmill compared to walking overground.8 These changes are suspected to be due to a combination of the proprioceptive input from the belt displacement, visual cues of the distance from the front of the treadmill, and the constant velocity of the belt.4,8
The use of rhythmic auditory cues, such as a metronome, can successfully improve gait mechanics in people with PD. Since individuals with PD have impaired motor automaticity, attentional control must be used to perform skills that were once automatic, like gait.6 External cues can successfully improve regulation of gait mechanics in people with PD.6 The theory supporting the use of auditory cues for improving spatiotemporal gait characteristics is that the cerebellar-thalamocortical circuit that is responsible for synchronization remains intact with PD and so rhythmic cues can improve the internal motor activation that is impaired.3 In practice, however, rhythmic auditory cuing has shown mixed results. Willems et al. examined the effects of metronome cues at various frequencies on overground gait mechanics in people with PD. They found that increased frequency resulted in increased cadence and gait velocity while decreased frequency of the metronome resulted in increased step lengths.9 Another study found similar results and concluded that increasing gait velocity should be the primary goal of treatment so metronome cueing should only be used at frequencies that match or are faster than the individual’s baseline cadence.10 They suggest that using decreased metronome frequencies may result in increased falls risk because it increases both step length and variability.10
Previous research has demonstrated there is a therapeutic benefit from walking on a treadmill for individuals with PD. The use of a metronome to provide auditory cueing is a frequent strategy used in gait training and most studies have investigated these effects with over ground walking. One study concluded that a combination of auditory and visual cues on the treadmill was more effective than the same cues used overground.11 They suggest that the treadmill provided an additional external cue that improved attention on gait and ultimately improved gait speed and stride cycle after treatment.11 To my knowledge, no study has investigated the immediate effects of metronome at various frequencies on the treadmill. Since a treadmill controls gait speed, changes in gait cadence can only be achieved by changing step length. When walking overground, changes in cadence can be achieved by changes in step length and/or gait speed. The purpose of this study is to determine the effect of metronome cues on spatiotemporal gait parameters when walking overground compared to walking on a treadmill in people with Parkinson’s Disease. This information will be critical in order to determine the optimal training environment to achieve specific gait training goals. I hypothesize that due to the inability to change the gait velocity on the treadmill, individuals with Parkinson’s Disease will have more significant changes in gait parameters when walking on the treadmill to metronome cueing than walking on the treadmill without cues or walking over ground with and without cues.
Methodology
Participants
Participants were recruited from the community via referrals from the Department of Neurology and from local Parkinson’s disease support groups. All participants were diagnosed with PD and had a Hoehn and Yahr (H&Y) Stage 1-3. Additional inclusion criteria included self-reported ability to walk >10 m over ground and on a treadmill for at least 14 minutes with rest breaks as needed. Exclusion criteria included H&Y Stage 4 and 5, uncontrolled cardiorespiratory/metabolic disease, other neurological/orthopedic disorders that affect gait, and severe communication impairments that impeded understanding of study purpose and procedures. Twenty-seven eligible participants were contacted and 21 agreed to participate. All participants were informed of the purpose and procedures associated with the study and signed an informed consent form approved by UNC-Chapel Hill.
Procedures
Participants were tested at the Human Movement Laboratory at the University of North Carolina-Chapel Hill. The Montreal Cognitive Assessment (MoCA) was administered for all participants to provide cognitive demographic data. A Unified Parkinson’s Disease Rating Scale (UPDRS) was administered to determine the stage of PD. To determine baseline gait speed, each participant walked over a 16 ft Zeno Walkway (Protokinetics, Haverford, PA) with instruction to walk at their “comfortable speed.” The Zeno software calculated baseline gait speed and cadence for every participant, which was used to determine the treadmill speed and metronome frequencies for the study.
Each participant performed 5 different trials of walking both overground and on a treadmill. The trials consisted of a baseline trial (no metronome) and 4 metronome trials of 85%, 90%, 100%, and 115% of the cadence calculated from the initial overground trial described above. The order of the metronome trials was randomized using a random number generator. The order of the treadmill and overground trials alternated between each testing subject. All participants wore a harness attached overhead, but no body weight support was provided and the harness did not restrict limb motion. Heart rate was monitored continuously using a pulse oximeter while walking on treadmill. The Google metronome was used and played through a speaker for all metronome trials.
Overground Testing
Each participant walked over the 16 ft Zeno Walkway 4 times for each testing condition. Instructions were given to “match each step to the beat of the metronome.” No assistive devices were used during these trials. The first initial steps of each trial and the turns between each walk were completed off of the walkway and were not included in the data collection. Standing rest breaks were given as needed in between trials.
Treadmill Testing
Participants walked on a dual-belt instrumented treadmill (Bertec Corp, Worthington, OH) for all treadmill trials. The treadmill speed was set at the baseline gait speed calculated from the initial overground trial. For three subjects, the treadmill speed was reduced due to inability to reach the intended treadmill speed safely. Participants were permitted to hold on to handrails if needed for balance but were discouraged from using them in order to promote more natural gait mechanics. Each testing trial lasted 1 minute. Rest breaks were given as needed. Oxygen saturation and heart rate were monitored for safety. Instructions were given to “match each step to the beat of the metronome.” A 1-minute baseline trial was performed first to allow for acclimatization to the treadmill before beginning metronome trials. Treadmill speed did not change throughout the duration of the treadmill trials. While participants walked on the treadmill, foot positions were tracked using markers on both heels and the Vicon Motion Capture system at 120 Hz. Ground reaction force data was also collected from the treadmill.
Data Management
For all overground trials, Prokinetic Software (pkmas) was used to collect data. This software removed partial steps and then automatically calculated step length, cadence, and gait speed from all remaining steps. For all treadmill trials, the Vicon system calculated step length by the anterior posterior distance between markers on each heel at heel strike. Cadence was calculated as the inverse of step time. Step time was calculated as every time heel strike occurred. A custom designed Labview Program was utilized to calculate outcome measures.
Data Analysis
SPSS version 24 was used for data analysis. Two-way repeated measures ANOVAs were used for step length and cadence. These were repeated for condition and environment. If significant main effects were found, paired sample T Tests were used as post hoc tests. Bonferroni correction was used for multiple comparisons. If significant interaction effects were found, one-way ANOVAs were used for each main effect. For cadence, one-way ANOVA was used to determine differences between environments and intended cadence at each target cadence. One-way ANOVA was also used for gait speed. A p-value of 0.05 was used for significance.
Results
Participants:
Twenty-one people with Parkinson’s disease participated in this study (13 male, 8 female; 69.8 ± 9.8 years old). The average MoCA score was 27 (± 2.9). The average time since onset of initial symptoms was 10.5 years (± 7.7 years). Five of the participants were classified as H&Y Stage 1, nine were classified as H&Y Stage 2, and seven were classified as H&Y Stage 3. The average UPDRS score was 19.4 (± 13.7). The average motor axial subscore was 4.8 (± 3.5). Nine were classified as axial rigid and 12 as tremor predominant.
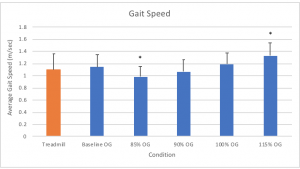
Gait Speed:
Gait speed was controlled on the treadmill for all trials. However, significant changes in gait speed were observed across conditions when walking overground (p<0.001, h2p=0.762). Gait speed significantly decreased for the 85% metronome condition (p=0.001) and significantly increased for the 115% metronome condition (p<0.001) compared to the baseline condition. There was a tendency to decrease gait speed for the 90% metronome condition (p=0.074). No significant change in gait speed was observed for the 100% metronome condition (Figure 1).
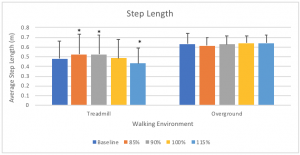
Step Length:
We observed a significant main effect for walking environment (p=0.003, h2p=0.362) with longer steps observed overground compared to on the treadmill. A significant interaction effect was observed between walking environment and metronome frequency (p<0.001, h2p=0.48). We therefore compared the effect of metronome frequency on step length on the treadmill and overground, separately. Here, we observed a significant effect of metronome frequency on the treadmill only (p<0.001, h2p=0.656), but not during overground walking (p=0.172, h2p=0.083). Post hoc testing of treadmill walking revealed that use of lower frequencies of metronome cues yielded significantly larger step lengths, with higher frequencies inducing smaller step lengths (Figure 2).
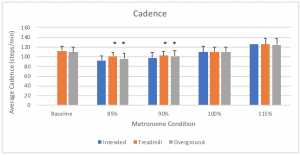
Cadence:
We observed a significant interaction for cadence between walking environment and metronome frequency (p=0.037, h2p=0.199). The interaction effect appeared to be due to the difference in cadence at 85% between treadmill and overground walking (p=0.006), whereas all other frequencies were not significantly different (all p>0.256). Given the significant interaction effect, we further assessed the effect of metronome frequencies for the treadmill (p<0.001, h2p=0.782) and overground (p<.001, h2p=0.903) environments separately. We were careful to include the intended frequency in our analyses as we sought to determine how well participants could reproduce targeted frequencies (Figure 3). We observed that for both the 85% metronome condition (p<0.001, h2p=0.426) and the 90% metronome condition (p=0.001, h2p=0.302) that cadence was significantly faster on both the treadmill and overground compared to intended cadence. Additionally, walking on the treadmill had significantly higher cadence at 85% compared to overground (p<0.001). There were no significant differences for the 100% or 115% conditions.
Discussion
My hypothesis that metronome cues on the treadmill would yield more significant changes in gait mechanics in people with PD compared to overground with and without metronome cues was partially supported. The optimal cueing and walking environment depends on the specific change in gait parameters desired. Specifically, for gait speed, metronome cueing at 85% and 115% overground yielded greater changes than all other trials. For step length, metronome cueing at 85%, 90%, and 115% on the treadmill yielded greater changes compared to all trials overground. In regards to cadence, participants had difficulty reaching the intended cadence for 85% and 90% metronome cues, however, walking overground yielded a greater decrease in cadence for those conditions compared to walking on the treadmill.
This study demonstrated that people with PD have the ability to change their gait in response to metronome cues both overground and on the treadmill. The mechanism underlying rhythmic cuing induced gait changes may lie in the ability to provide external regulation of rhythmic timing. Importantly, functional magnetic resonance imaging (fMRI) studies have demonstrated diminished activation in many locomotor areas of the brain that control timing of gait in people with PD.12 This altered activation impairs the ability to independently modify gait mechanics through internal regulation3. By providing external cues, like the metronome and treadmill, less demand is placed on internal regulation of gait. Since the motor circuits for synchronization remain intact, the use of treadmill and rhythmic auditory cues should improve gait mechanics in ways the person would not be able to change and maintain independently.4,8–10 Our results supported this theory demonstrated by the changes observed in gait speed, step length, and step cadence in response to the metronome cues and walking environment.
This study also demonstrated that treatment must be specific to the desired goal. Treatment plans must be designed to promote the ultimate goal of treatment based on available evidence, clinician knowledge, and experience. It is critical that treatment matches the desired goal. When developing a treatment strategy, a hypothesis should be formulated that the chosen treatment plan will achieve the desired outcome.13 Common gait abnormalities in people with PD include decreased gait speed, decreased step length, and increased cadence.3–5 Therefore, treatment goals often include increasing gait speed, increasing step length, and decreasing cadence. Based on the results from this study, to increase gait speed, walking overground with the 115% metronome cue is the only treatment option that produced increased gait speed. If the goal is to increase step length, walking on a treadmill with 85% or 90% metronome cues is the only treatment option that promoted larger step length. To decrease cadence, the 85% and 90% metronome cues must be used either overground or on the treadmill, however, overground resulted in a greater reduction of cadence compared to the treadmill at these frequencies.
This study also demonstrated that the frequency of the cue provided is more important than the person’s ability to successfully match the cue. Participants in this study were only able to accurately match their step with the 100% and 115% metronome cues both overground and on the treadmill. Although they were unable to match the 85% and 90% cues, those conditions still produced significant changes in spatiotemporal gait mechanics. Thus, even when the cue is not accurately matched, the desired gait changes can still be observed.
There were several limitations to this study. First, some participants used the handrails on the treadmill and some did not. In healthy adults, the use of handrails when walking on a treadmill significantly decreases step length and width variability but not step time variability.14 Not surprisingly, step variability increases when walking without handrails in people with PD.4 This is likely because handrails provide support for improved balance and mobility.4 In healthy adults, there is no significant difference in step length found between holding or not holding handrails on treadmill.15 Most untrained people, especially those with PD, require handrails to safely perform treadmill walking and many studies do not report whether handrails were used.4 Although gait variability was not one of the outcomes assessed in this study, there is potential for differences in gait mechanics depending on use of handrails. There was also potential for fatigue-related changes in gait since no rest breaks were given unless the patient requested one or heart rate or gait quality indicated the need for one. Lower extremity fatigue in PD impacts gait parameters including step length and gait speed.16 Finally, there were more people with stage 2 and 3 PD than stage 1, so these results may be more heavily influenced by more advanced PD.
In conclusion, I observed a significant relationship between frequency of metronome cues and walking environment for gait mechanics in people with PD. The desired gait change (i.e. gait speed, step length, or cadence) directly influences the type of cue and environment used in order to achieve that goal. People with PD are able to successfully change their gait speed, step length, and cadence in response to these conditions; however, further exploration is needed to determine if these results can used as a gait training technique that carries over to long-term gait changes.
References
- de Lau LML, Breteler MMB. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006;5(6):525-535. doi:10.1016/S1474-4422(06)70471-9.
- Bereczki D. The description of all four cardinal signs of Parkinson’s disease in a Hungarian medical text published in 1690. Parkinsonism Relat. Disord. 2010;16(4):290-293. doi:10.1016/j.parkreldis.2009.11.006.
- Rodger MWM, Craig CM. Beyond the Metronome: Auditory Events and Music May Afford More than Just Interval Durations as Gait Cues in Parkinson’s Disease. Front. Neurosci. 2016;10:272. doi:10.3389/fnins.2016.00272.
- Bello O, Fernandez-Del-Olmo M. How does the treadmill affect gait in Parkinson’s disease? Curr. Aging Sci. 2012;5(1):28-34.
- Nombela C, Hughes LE, Owen AM, Grahn JA. Into the groove: can rhythm influence Parkinson’s disease? Neurosci. Biobehav. Rev. 2013;37(10 Pt 2):2564-2570. doi:10.1016/j.neubiorev.2013.08.003.
- Wu T, Hallett M, Chan P. Motor automaticity in Parkinson’s disease. Neurobiol. Dis. 2015;82:226-234. doi:10.1016/j.nbd.2015.06.014.
- Keus SHJ, Bloem BR, Hendriks EJM, Bredero-Cohen AB, Munneke M, Practice Recommendations Development Group. Evidence-based analysis of physical therapy in Parkinson’s disease with recommendations for practice and research. Mov. Disord. 2007;22(4):451-60; quiz 600. doi:10.1002/mds.21244.
- Bello O, Marquez G, Camblor M, Fernandez-Del-Olmo M. Mechanisms involved in treadmill walking improvements in Parkinson’s disease. Gait Posture 2010;32(1):118-123. doi:10.1016/j.gaitpost.2010.04.015.
- Willems AM, Nieuwboer A, Chavret F, et al. The use of rhythmic auditory cues to influence gait in patients with Parkinson’s disease, the differential effect for freezers and non-freezers, an explorative study. Disabil. Rehabil. 2006;28(11):721-728. doi:10.1080/09638280500386569.
- Arias P, Cudeiro J. Effects of rhythmic sensory stimulation (auditory, visual) on gait in Parkinson’s disease patients. Exp. Brain Res. 2008;186(4):589-601. doi:10.1007/s00221-007-1263-y.
- Frazzitta G, Maestri R, Uccellini D, Bertotti G, Abelli P. Rehabilitation treatment of gait in patients with Parkinson’s disease with freezing: a comparison between two physical therapy protocols using visual and auditory cues with or without treadmill training. Mov. Disord. 2009;24(8):1139-1143. doi:10.1002/mds.22491.
- Peterson DS, Pickett KA, Duncan RP, Perlmutter JS, Earhart GM. Brain activity during complex imagined gait tasks in Parkinson disease. Clin. Neurophysiol. 2014;125(5):995-1005. doi:10.1016/j.clinph.2013.10.008.
- Ingram BL. Chapter 1: A Framework for Clinical Case Formulations. In: Clinical Case Formulations: Matching the Integrative Treatment Plan to the Client . 2nd ed. John Wiley & Sons, Inc; 2012:3-18.
- Owings TM, Grabiner MD. Variability of step kinematics in young and older adults. Gait Posture 2004;20(1):26-29. doi:10.1016/S0966-6362(03)00088-2.
- Siler WL, Jorgensen AL, Norris RA. Grasping the handrails during treadmill walking does not alter sagittal plane kinematics of walking. Arch. Phys. Med. Rehabil. 1997;78(4):393-398.
- Santos PCR, Gobbi LTB, Orcioli-Silva D, Simieli L, van Dieen J, Barbieri FA. Effects of leg muscle fatigue on gait in patients with Parkinson’s disease and controls with high and low levels of daily physical activity. Gait Posture 2016;47:86-91.
PDF of manuscript:
Self-Reflection
This research experience was extremely rewarding for me as a person, student, and future PT. I now have a much better understanding of the research process from designing and conducting the study, to analyzing results, and finally drawing conclusions and presenting the results. I have also improved my knowledge of gait and strategies to improve gait in people with PD. Over the course of these past 2 semesters, I have been challenged in numerous ways in an environment that has ultimately fostered improved critical thinking and reasoning skills which will better prepare me for beginning my PT career. The relationships I have developed with my entire research team have provided outstanding mentorship that I will forever be thankful for. Having only one prior research experience, I was unsure of what to expect with this project and I am so glad I chose to be involved in this opportunity.
Image sources: https://www.today.com/health/6-fat-burning-treadmill-workouts-you-will-love-t10421 and https://www.shareicon.net/metronome-tempo-music-beat-764576


4 Responses to “The Effects of Metronome Frequency and Walking Environment on Gait in People with Parkinson’s Disease”
Michael Lewek
Maddie
I’m very proud of the job that you and Guneet did on this project. As we already discussed, these data are already serving as critical preliminary data for a grant application. I look forward to having this out in publication so your contribution can be shared with others. Great job.
Mike
Maddie Wygand
Thank you Hailey and Ned for the comments! I am glad you both found value in the results of this study. Like you, I am also looking forward to seeing what next steps may come out of this in order to continue to better understand how we, as PTs, can better perform gait training in this patient population!
Ned Bixby
Hi Maddie,
I too have had family experiences with PD. My grandfather had PD and still lived till he was 92! During the course of his disease he had many physical therapy sessions which focused on improving his gait. He presented with the typical gait pattern of decreased speed, decreased step length, and increased cadence. The research you conducted and have presented to us is really interesting. It is great to see that people with the disease are able to change their gait pattern and pace when provided external auditory cuing. I would love to see how this would translate to their typical walking outside of the clinic after being treated for a few weeks, but your study has laid the ground work for that to be the next step. To now have the knowledge and evidence that certain metronome cues will impact the patient’s gait in different ways, I can definitely see this being used as an intervention to improve a patient’s speed, step length, and/or cadence.
Amazing job Maddie!
Hailey
Maddie, I’m thoroughly intrigued by your capstone project interest and am impressed with all of the work you have completed! While attending your presentation yesterday, it was absolutely amazing to hear about the potentially groundbreaking discoveries that y’all found! I was especially impressed with the fact that you were able to show one of your participants that he was in fact able to change his walking cadence, a fact that he himself believed to be untrue. I anticipate seeing major breakthroughs in the treatment of Parkinson’s disease, with you as a contributor! Once again, great project and I can’t wait to hear about your successes as a future PT!
-Hailey