Anterior Cruciate Ligament Reconstruction: Part 1 – Surgical Considerations, Grafts, & Healing
Angela Lauten, SPT
Introduction
Well hello there folks and welcome to my Capstone website! My interest in the ACL has sort of a one-thing-led-to-another kind of story. I have not personally experienced this kind of injury, as my Co-Capstone buddy (Kyle Hoppes) has, but being a competitive gymnast for 16 years, I was definitely exposed to ACL tears amongst my teammates. However, it was not until I was on a clinical rotation during my 2nd year that my interest in this particular injury was sparked. After learning about ACL injury and reconstruction in our Musculoskeletal II class, I observed some rehab techniques during this clinical rotation that 1) I was unfamiliar with and 2) I wasn’t sure I agreed with. As a result, I sought out the literature and gave an inservice on the topic of ACL graft types and basic rehab considerations. Then, in our Evidence-Based Practice II class, I decided to delve a little deeper into the topic, specifically trying to answer the following PICO question: In middle-aged, active individuals status post ACLR, does an allograft or autograft lead to better return to premorbid activity levels? Even after writing a whole research paper (don’t worry, I’ll just provide the summary for you here), I still wasn’t satisfied with the information I’d found. Thus, the research for this Capstone presentation has centered largely around understanding all the factors that play into the ACLR rehabilitation process: What factors may have predisposed this patient to ACL injury? What is the anatomy/physiology of the native ACL and its biomechanical roles and properties? What are the options for ACLR graft selection and their associated advantages/disadvantages? What are the biomechanical properties of various grafts and why do we need to know this for rehab? How does the graft tissue heal and how does this vary from autograft to allograft or with bone-to-bone fixation versus soft tissue-to-bone fixation? What other patient-related and rehab factors must we consider for the healing of the tissue and a safe return to activity or sport?
Collaboration
Because I wanted to understand the full spectrum of ACLR, I decided to collaborate with my classmate, Kyle Hoppes. His research over the last year has looked at the more advanced side of the rehab process – he has scoured the literature to look at accelerated versus non-accelerated protocols, return-to-play criteria, various outcome measures, and has done an excellent job to provide further evidence that we need to be critical thinkers and tailor each piece of intervention to the individual. Just as no 2 patients are the same, no 2 ACL reconstructions are the same either. I think I can speak for both of us when I say that we never want to just follow a protocol simply because it is given to us – rather, we want to understand the injury, the surgery, the individual’s goals and desires, and how and why this dictates the rehab process.
Products and Pertinent Findings
As a result of our collaborative process, Kyle and I produced a Voicethread module intended for students and faculty. If you click on this link, you will automatically be added to “Kyle & Angela’s Capstone Group.” If you have clicked on the “My Voice” tab, you should see this group listed, and you should be able to view our voicethread entitled “ACLR Capstone.” However, if you find yourself just wanting to look at the slides, then you are free to do that as well. Additionally, we have each created a handout based on the specific research we did. You may access my handout here, and I would encourage you to head over to Kyle’s Capstone page and grab a copy of his handout! Furthermore, if you’re interested in any of our literature, we have provided a combined reference list for your perusing pleasure.
From my new literature search on the anatomy/physiology of the native ACL, biomechanical properties, graft types, and healing properties of these tissues, here are some little nuggets of information you can add to your think-tank:
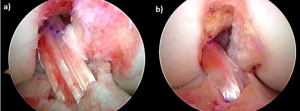
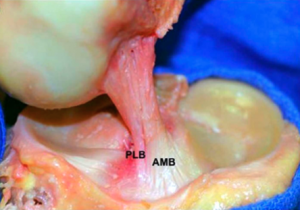
- The native ACL has been recognized to have at least 2 bundles: an anteromedial (AM) and a posterolateral (PL) bundle. You may, however, come across literature that makes a case for a 3rd portion, called the intermediate bundle. The distinction between bundles is important because each plays a different kinematic role: the AM bundle is more taut in knee flexion (>90deg) and the PL bundle is more taut in knee extension (<30deg). As such, if the surgical reconstruction does not aim to conform to the patterns born by the native bundles, this could potentially contribute to post-ACLR laxity or a different distribution of forces across the graft or the knee joint. (Gabriel et al, 2004)
- The ultimate goal of ACLR is to restore ACL function and normal knee joint kinematics – however, this can be affected by graft selection, graft fixation, and the rate of tissue healing. (Yabroudi & Irrgang, 2013)
- Selecting the right graft for the individual depends on several factors: patient preference, age, activity level, physical requirements, expected outcomes, timeline for return to play, concomitant injuries, previous ACLR, tissue availability, and surgeon preference/experience. (Vyas et al, 2012)
- Each graft type, whether allograft or autograft, bone-patellar tendon-bone (BPTB), hamstring tendon (HS), or otherwise, has its own advantages and disadvantages. Please refer to my handout for a nice reference chart of these advantages/disadvantages.
- When a new graft has stress placed upon it, this load is also born by the tibial and femoral fixation points. In the early post-op period (~6-8wks), the fixation sites are often the weakest link, not the graft itself. It’s important to keep in mind that as we intentionally place various stresses across the joint during the rehab process, the graft and the fixation devices are being loaded. (Dargel et al, 2007; Brand et al, 2000)
- All grafts undergo a sequential process of healing and ligamentization: 1) Inflammation and graft necrosis (lasts 1-2mos after surgery); 2) Revascularization and cell repopulation (20days to 6mos after surgery); 3) Remodeling (12-18mos after surgery). (Baer & Harner, 2007)
- Biologic healing and incorporation of grafts require time! No rehab protocol has been shown to change the time to graft healing and maturation. Therefore, advance your interventions with consideration for tissue healing and the individual’s response! (Escamilla et al, 2012; Vyas et al, 2012)
Evaluation of Materials
As our voicethread and handout materials are intended to be a resource for students, we sent our committee members this evaluation form so that we might make any necessary changes before making it available to you all! Additionally, our voicethread may be used as a supplemental teaching module for the Knee Unit in the Musculoskeletal II class, so Kyle and I did our best to incorporate the immediate feedback from our committee members into our voicethread and handouts. We would also love to hear your feedback for our presentation – so if you get a chance to see it, please feel free to fill out our evaluation form, and send it to us: kyle_hoppes@med.unc.edu, alauten@med.unc.edu
Kudos and Thanks
I’d like to extend some major gratitude to the following people: Kyle Hoppes (for being an amazing Co-Capstone buddy – you rock!), Mike Gross (our advisor; for helping me dig deeper into tissues, for being a Voicethread guru, and for responding so quickly to all amounts of logistical/please-help-me emails), Jon Hacke (committee member; for your prompt and thorough feedback, for early conversations about what our Capstone could be, and for wanting to use our information to supplement the MSKII class), James Massey (committee member; for meetings at Starbucks, for additional resources, and for encouraging and super helpful feedback), and Mike McMorris (for taking the time out of your busy schedule to brainstorm ideas with me, and for helping me narrow down and organize my ‘boxes’, both in EBPII and throughout this whole Capstone process).

2 Responses to “ACL Reconstruction: Part 1 – Surgical Considerations, Grafts & Healing”
Mike Gross
Angela- Excellent work on all phases and end products for this project. It is easy to see that you and yle learned a lot in the process and accomlished your goals and more for the work that you all did. Fantastic. Mike Gross
mlchrist
Hi Angela!
First I have to say, you and Kyle have done an awesome job of combining your two parts of the project for a very comprehensive look at all the stages of ACL injury & rehab!! I listened to a little bit of the voicethread (and want to hear the rest once I have more time), and think it will be a good resource for the Musculo II class. Your slides are clear and concise, and your voice-over adds in the details at a nice speed for your listeners. Accessing the voicethread turned out to be tricky – every time I clicked on “My Voice,” the website told me that I had “already been added to Kyle & Angela’s Capstone group,” but did not take me to the actual presentation (I managed to find my way to the presentation once, but have not been able to get back since). This might be a glitch in the website (so I’ll check back later) or it might just be me struggling with technology… either way, just wanted to give you a heads up that there might possibly be a problem with access.
I like all the colors in your handout! Very eye-catching, and a great summary of the topics you cover in your presentation. I would love to be able to save a copy for future reference (if that’s ok with you?). The quick comparison of graft types is especially helpful, and the “Key Factors that Influence Outcome” section right below it is a nice reminder for intervention planning too.
Your explanation of the different bundles in the “native ACL” definitely grabbed my attention. I had never stopped to consider the structure of the ligament before, but given the fact that it helps to control so many motions at the knee joint, the presence of multiple bundles makes a lot of sense. I feel as though this knowledge could also come into play when planning intervention. I wanted to go back and listen to your voicethread commentary on the bundles, however this is the point at which I found that I could not get back to the presentation … I’ll try again later 😛
As you point out, attention to the individual patient and not simply to a general protocol is far more likely to increase the success of rehabilitation and recovery. Your desire to understand how various factors affect ACL injury, surgery, and recovery is clearly evident in the fantastic level of detail you have presented! Great work with this project, and thank you for sharing what you’ve found. Good luck with your last rotation! ~ Megan C.