Lower Extremity Functional Electrical Stimulation Cycling Training in Rehabilitation Post Stroke and Spinal Cord Injury
by Brandon Lindquist
[youtube]http://www.youtube.com/watch?v=KGfjkDAJ40w&list=PL7AA3B9D92429123A&index=2[/youtube]
Introduction
During a clinical rotation at a skilled nursing facility (SNF) I was introduced to patterned electrical neuromuscular stimulation (PENS). The Accelerated Care Plus (ACP) Corporation recommends PENS use in the acute and subacute phases of incision healing to keep the affected muscles conditioned, to manage inflammation, and to prevent muscle contracture, as research has demonstrated PENS’s effectiveness for muscle re-education and treatment of muscle disuse atrophy following trauma, injury, or surgery. The ACP Corporation also states that PENS devices may be used to assist in the treatment of symptoms of neuromuscular disease, including stroke.
I used PENS in an attempt to help improve quadriceps, hamstrings, tibialis anterior, and gastrocnemius muscle contractility with a patient in the subacute phase post stroke and as a future evidence-based practitioner I wanted to find out if there is evidence to support PENS use for this purpose. I found a randomized, controlled trial reporting that 30 minutes of PENS use, simulating a pattern of walking, plus 1 hour of standard rehabilitation is more effective than 1 hour of placebo PENS, plus 1 hour of standard rehabilitation at increasing overground walking ability when performed 5 days per week, for 3 weeks.35 However, I found the research design to be questionable, as the treatment group was being provided with an added amount of active therapy compared to the control group.
I wanted to find an intervention with convincing evidence of improving overground walking ability with stroke patients that involved neuromuscular electrical stimulation (NMES). In my searching I came across functional electrical stimulation cycling (FESC) as a method of rehabilitation for patients with neuromuscular impairments caused by stroke.
Over the course of the Evidence-Based Practice (EBP) II course, I found evidence that incorporating brief sessions of FESC into a rehabilitation program with patients who have suffered a hemiparetic stroke, both in the subacute phase9 and in the chronic phase8, promotes overground ambulation recovery. However, it has not demonstrated being any more effective than standard rehabilitation (SR) methods (e.g., stretching, muscular conditioning with active and/or passive mobility, sitting and standing balance training, and gait training) in improving objective measures of walking recovery (e.g., gait speed).13,17 Nonetheless, this information demonstrates that there are alternative, and potentially safer approaches that can be used to achieve improved overground walking ability. Additionally, when used in the subacute phase: advantages in improving motor control8,9, and reducing muscle tone and spasticity15,36 are evident, when compared to SR; and in a subgroup of this population who are too impaired to perform SR efforts, FESC has the potential of expediting the time to overground ambulation recovery and/or improving long-term walking ability.9
Project Overview
Compared to overground gait training, supervised or assisted by a physical therapist (PT), FESC training has the potential of protecting PTs against unnecessary injury that can impact the length of time a PT can practice and their future quality of life (QoL). As such, FESC is worth considering for use in clinical practice. Therefore, I have developed an online presentation and handout to deliver to entry level students about FESC trainings potential in the rehabilitation process with patients post hemiparetic stroke. Additionally, I have decided to expand the information presented to patients affected by spinal cord injury (SCI). The presentation outlines: a description of FESC; indications for, contraindications to, and precautions when using FESC; a typical FESC protocol; barriers to implementing FESC into clinical practice; and reimbursement for FESC use. The handout includes a condensed version of the information in the presentation that is meant to act as a quick reference when using FESC in clinical practice. A literature review of the evidence used to develop this project is also included at the end of this document. Lastly, I have attached an evaluation form at the end of the presentation. This can be filled out by students who review the online presentation and handout materials to provide feedback about the content included within this presentation
I would like to provide special thanks to my committee members, Kathleen Lovell and Patty Creatore, who provided me with very helpful feedback along the course of developing this capstone. I would also like to thank my faculty advisor for this project, Karen McCulloch, who provided me with both guidance and feedback along the way.
Presentation
Learning Objectives
By the end of this presentation, the learner will be able to:
- Describe what functional electrical stimulation cycling (FESC) is, including equipment needed for its implementation into clinical practice.
- Identify contraindications/precautions for using FESC.
- Identify indications for using FESC with persons affected by impairments and functional limitations related to stroke or spinal cord injury (SCI), including mechanisms for improvements.
- Describe a typical FESC protocol that can be used with persons affected by impairments and/or functional limitations related to stroke or SCI.
- Identify barriers to implementing FESC into clinical practice.
- Describe how FESC is billed.
Description of and Primary Complications Post Stroke/Cerebrovascular Accident (CVA)/Brain Attack
- Stroke occurs when a blood clot blocks the blood supply to part of the brain or when a blood vessel in or around the brain bursts, resulting in brain damage or death.1
- Primary complications post stroke vary depending on the location, type and severity of the stroke, but can include impaired sensory, motor, and/or cognitive functions.2
- Persons who have suffered a stroke often have:2
- Areas of decreased or absent sensation and/or motor control.
- Spastic muscle tone.
- Difficulty walking.
- Difficulty speaking or understanding speech.
- Difficulty seeing.
Description of and Primary Complications Post Spinal Cord Injury (SCI)
- SCI most often occurs when the spinal cord is damaged by a traumatic incident, but can also occur as a result of spinal cord ischemia (usually associated with cardiovascular disease) or spinal cord compression from various diseases (e.g., infections, cancers, etc.).3
- Primary complications post SCI include:4
- Decreased or absent sensory input (e.g., proprioception).
- Decreased or absent motor control.
- Spastic muscle tone (usually bilaterally).
Secondary Complications Post Stroke
- Persons who have had a stroke are at a more than 40% increased risk of having a recurrent stroke within 5 years, which can be attributed to continuation or worsening of dysfunctional lifestyle choices (e.g., smoking, poor diet, low levels of physical activity, and alcohol abuse) and mismanagement of other stroke risk factors (e.g., hypertension, diabetes and heart arrhythmias).2
- Persons with impairments and functional limitations related to stroke are more likely to have non-adapted activity and participation restrictions, and therefore reductions in self-perceived quality of life (QOL).5
Secondary Complications Post SCI
- Urinary tract infections (UTIs) (leading cause of rehospitalization).6
- Pressure ulcers (more likely in persons with T1-S5 SCI).6
- Autonomic dysreflexia.7
- Pneumonia/atelectasis (more likely in persons with C1-C8 SCI).6
- Deep venous thromboses (DVTs).7
- Similar to persons affected by stroke, persons affected by impairments and functional limitations related to SCI are also more likely to have non-adapted activity and participation restrictions, and therefore reductions in self-perceived quality of life (QOL).
Considerations for Rehabilitation Post Stroke or SCI
- Rehabilitation strategies should be:8
- Effective at reducing impairments, improving function, improving fitness, and/or avoiding secondary health complications.
- Safe.
- Practical.
- As functional as possible.
- Functional electrical stimulation cycling (FESC) training should be considered for use in rehabilitation post stroke or SCI as it is:
- Robust in improving structural and functional status.
- Safe for persons who are too impaired to attempt gait training efforts.
- Practical as a transitional tool or adjunct to other, more functional rehabilitation efforts, as it simulates the functional act of walking.
Description of FESC

- FESC is the use of neuromuscular electrical nerve stimulation (NMES) to coordinate activation of the lower extremities (LEs) in sync with the cycling movement, which approximates the cyclic movement of walking.9
- FESC can be most easily accomplished using a Restorative Therapies (RT)300-SL FES/motor powered leg cycle ergometer (Restorative Therapies, 1434 Fleet Street, Baltimore, MD, 21231 USA), which:10
- Is the only commercially available FESC system.
- Many investigators in the reviewed studies on FESC fashioned their own systems, so it is possible to make your own, but that would come along with a variety of other provisional requirements for use approval.
- Has an integrated multi-lead electrical stimulation (ES) unit that has the ability to synchronously stimulate up to 10 muscle groups of the LEs and trunk (5 muscle groups on each side of the body) to the cycling motion.
- Is able to:
- Provide dynamic ES, resistance and motor support based on cycling smoothness (i.e., presence of spasticity), performance and the phase of the cycling session (i.e., warm-up, active and cool-down phase).
- Display real time performance information (e.g., power output, symmetry, ES level, speed, distance, pulse rate, and oxygen saturation).
- Record multiple pieces of performance facts (e.g., average energy expenditure, distance, average ES intensity, and peak and average pulse rate).
- Initiate the cool-down phase automatically if the user falls below a preset cadence, pulse rate or oxygen saturation, or above a preset pulse rate (i.e., if the user becomes fatigued).
- Is the only commercially available FESC system.
Indications for Using FESC
A complete literature review on indications for using FESC is available at the end of this presentation, including possible mechanisms of improvements in the given areas.
Subchronic (i.e., 5-90 days) Stroke:
- LE muscle weakness.13
- LE spastic muscle tone.14,15,16
- Limited overground walking ability.9
Chronic (i.e., > 90 days) Stroke:
- LE muscle weakness.17
- LE muscle fatigability.8,17
- LE spastic muscle tone.18,16
- Limited overground walking ability.8
Chronic Motor Incomplete SCI:
- LE muscle weakness.19,20
- LE muscle fatigability.12,20
- Glucose intolerance.12
- Presence of biochemical inflammatory markers associated with heart disease.12
- Limited overground ambulation ability.20
Chronic Complete SCI
- FES-induced LE muscle weakness.21
- FES-induced LE muscle fatigability.12,21
- LE spastic muscle tone.22
- Glucose intolerance.12
- Presence of biochemical inflammatory markers associated with heart disease.12
Contraindications to Using FESC11,12
- Skin breakdown that limits the ability to sit for prolonged periods.
- Skin irritation at the site(s) of electrode placement.
- Cardiovascular, pulmonary or cardiopulmonary disease without clearance from the PCP.
- Implanted cardiac pacemakers or defibrillators.
- Implanted metal instruments, vasomotor instability, heterotopic ossification, unhealed or recent bone fractures, or neoplasm in any of the areas being stimulated.
- Pregnancy.
- Epilepsy.
Precautions when Using FESC11,12
- Lower motor neuron injury.
- Limited ROM of the involved joint(s).
- Decreased sensation.
- Osteoporosis.
- Joint instability.
- Frequent or severe bouts of autonomic dysreflexia.
- Cognitive issues that prevent the individual from communicating a problem during stimulation.
Implications of FESC for Clinical Practice
- In persons with subchronic or chronic stroke, or chronic SCI, FESC training has proven to be not only effective, but at least as effective as other training methods (i.e., standard rehabilitation and nonassisted cycling training) at:
- Increasing LE muscle strength.
- Reducing LE spastic muscle tone.
- Improving overground ambulation ability (when applicable).
- FESC training potentially has advantages over other training methods, including gait training, when it comes to improving functional mobility, as it has been shown to:
- Enhance reductions in spastic muscle tone in all reported populations, with the exception of persons with chronic motor incomplete SCI18,14,15,22,16
- Enhance improvements in motor control in persons with subchronic stroke, which has implications for reducing falls risk.13
- Enhance improvements in glucose tolerance and reductions in biochemical inflammatory markers, which has implications for reducing risk of developing cardiovascular disease.12
- Compared to gait training, cycling training creates a safer environment for both the patient (reduces risk of injury from falling or excessive handling) and the treating therapist, especially in cases where the patient has severe motor loss or other complications that necessitate extensive assistance.8
FESC Protocols
[youtube]http://www.youtube.com/watch?v=glH5E66sr0o[/youtube]
Note: The below protocols are a general guideline. In reality, setup will be patient specific, as people may respond differently to different setups. Additionally, depending on the cognitive status of the user, the ES and ergometer setup can be performed very easily independently. Once setup becomes familiar, it should take no more than 10 minutes.
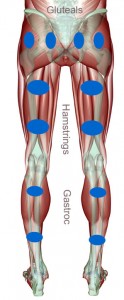
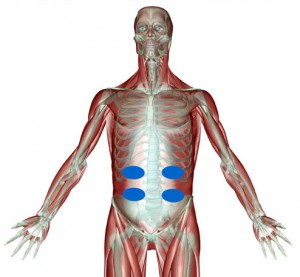
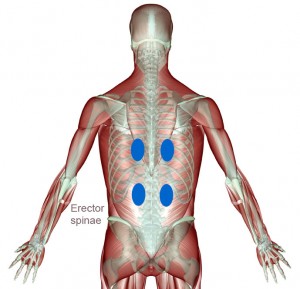
ES Setup:12,23,21
- If FES-induced cycling (IC) training is being used, place electrodes on bilateral gluteals, quadriceps and hamstrings muscles, and if desired on the triceps surae and/or tibialis anterior muscles.
- If FES-assisted cycling (AC) training is being used, place electrodes on the specific muscle groups that the individual user is lacking control over.
- Set the waveform to biphasic or sinusoidal.
- Set pulse duration to 500 μs.
- Set pulse frequency to 20, 30, or 50 Hz, depending on muscle endurance (lower frequencies decrease fatigability).
- Current intensity is usually adjusted automatically by the ES unit within user tolerated parameters, which should not exceed 70 mA at the tibialis anterior or 140 mA at any other LE muscle group.
Ergometer Setup: (based on the RT300)
- Pull the user up to the ergometer in a sturdy chair (a wheelchair is commonly used) and anchor the chair to the ergometer (anchors are located on the bottom of the RT300).
- Strap the users legs into the AFO-like pedals.
- Start the ergometer.
- The ergometer will initiate the warm-up period, which starts with a period of passive motor (M)-IC.
FESC Training Parameters:
- Set cycling cadence at or above 35 rpm to user preference.
- The cycling cadence is achieved through some combination of ES current intensity and cycling resistance.
- Set pedal resistance to a level that can be performed for at least 10 consecutive minutes in the first cycling interval.
- As the rehabilitation program continues the resistance should be progressed based on user capacity.
- If the user is able to complete more than 10 consecutive minutes in the first cycling interval or for 3 consecutive training sessions, the resistance should be increased by 1 kp at the next session.
- If a given increase in resistance results in excessive spastic muscle tone production, the resistance should be decreased to a tolerated level and attempted to be increased again at the next training session.
- As the rehabilitation program continues the resistance should be progressed based on user capacity.
- If the user is unable to produce enough power to sustain the cycling motion above a 35 rpm cadence at the maximum tolerated current intensity and 0 kp pedal resistance for 10 consecutive minutes, an acclimation period of NMES should be performed before continuing FESC training (see below).23
- The user should complete no more than 8 FESC intervals per training session.
- The RT300 automatically initiates a 5 minute M-IC rest period if the user drops below a cadence of 35 rpm.
- After 8 FESC intervals the RT300 automatically initiates a cool-down regardless of reaching the target session duration or not (usually 2 mins of M-IC, but can be adjusted if a longer cool-down is desired).
- Training frequency should be anywhere between 2-5 sessions per week.
- Session duration should be between 10 and 60 minutes.
- The duration of the rehabilitation program will vary depending on progress toward goals or on achievement of all goals.23,12,21
- FESC units are available to purchase for personal use and are commonly purchased by users after completing a rehabilitation program, so as to maintain or further gains.
NMES Acclimation Period Parameters:23
- ES setup is the same as that used for FESC, with the exception of using an on:off cycle (seconds) of 6:2 for each muscle group.
- Resistance should be progressively increased by adding weights to the ankle in 1 kg increments.
- Training frequency should be 3 days per week.
- Session duration should be targeted at 30 minutes for each muscle group per session.
- 5 minute rest periods should be initiated when no muscle contractions are visible during NMES training.
- Once FESC can be sustained for 10 consecutive minutes, as determined by weekly attempts, the individual can be started on the FESC training protocol (see above).
Barriers to Implementing FESC into Clinical Practice
- Although setup time is relatively minimal, time required for application and removal of electrodes, and assisting the individual with setup and takedown could cut into therapy time.
- Cost of purchasing and maintaining the specialized equipment and accessories.
- The price of a RT300-SL is $20,500 for clinical purposes, which increases if you want a system that has an added arm ergometer, but includes training and support24, which is quite the investment for a physical therapy operation.
- The price of a RT300-SL for an individual user, if purchased for home use, is $16,400 for a system with training and support.24
Reimbursement for FESC
- Medicare does reimburse for use of FESC training with persons recovering from stroke and SCI.
- ES can be billed for up to 10 minutes/session, which can only include time for setup and take down, and for a skin check.
- CPT code: G0283
- Depending on the goal of its use, FESC can be billed for the amount of time spent in the activity as either Therapeutic Activity (CPT code: 97530) or Therapeutic Exercise (CPT code: 97110).
- ES can be billed for up to 10 minutes/session, which can only include time for setup and take down, and for a skin check.
Literature Review of Indications for Using FESC
LE Muscle Weakness
A period of FESC training effectively improves quadriceps muscle strength in persons with subchronic13 or chronic17 hemiparesis post stroke, or chronic paraparesis19,20 or paraplegia21 post SCI. Mechanisms of improved muscle strength after a period of FESC training may include: an increase in neural drive to and/or improved central control of CNS-connected muscle fibers; an increase in rate of motor unit firing leading to increased tension development; an increased probability of doublet firing in individual motor units; improved motor unit synchronization; and/or central control of training-related adaptation to resistive exercise.25
In persons with subchronic hemiparesis post stroke, Ferrante et al13 reported a statistically significant, 10 times greater mean increase in hemiparetic quadriceps strength after 4 weeks of FES/M-IC training performed 7 days per week for 35 minutes per session, as compared to a time matched rehabilitation program that similarly included stretching, muscular conditioning, active and passive range of motion, trunk control exercises, standing exercises, and gait training, but not FES/M-IC.
In persons with chronic hemiparesis post stroke, Janssen et al reported a statistically significant, 7.4% mean increase in hemiparetic quadriceps strength after 8 weeks of FES-AC training that produced continuous muscle overload, performed 3 days per week for 30 minutes per session. These investigators also included a control group who performed time matched nonassisted cycling training and achieved statistically similar results.17
In persons with chronic paraparesis post incomplete SCI, defined as American Spinal Injury Association (ASIA) classifications of B, C, or D, Liu et al reported a statistically significant mean increase in right (R) knee extensor, and R and left (L) knee flexor strength of 14.6%, 10% and 11.9%, respectively, and a non-statistically significant mean increase in L knee extensor strength of 2.6%, after 8 weeks of FES-IC training performed 3 days per week for 30 minutes per session.19 Additionally, in a case study by Donaldson et al20 a single individual with chronic incomplete SCI causing hemiparesis of the R LE, was reported to have improved the strength of his quadriceps muscle by 45.8% after 16 months of FES-AC training, performed for an average of 21 minutes per day. However, this is an extremely underpowered report that needs to be investigated further using a more highly powered study design.
In persons with chronic paraplegia post incomplete SCI, Duffell et al21 reported a statistically significant mean increase in ES-induced L quadriceps strength of 399% and 673%, after 3 months and 12 months, respectively, of FES-IC training performed 5 days per week for up to 30 minutes per session. Additionally, in the same individual mentioned above who also had chronic hemiplegia of the L LE, it was reported that he recovered volitional quadriceps strength (went from not being able to produce any torque to being able to produce torque of 34 Nm) that enabled him to move his L leg when it became uncomfortable.20
LE Muscle Fatigability
A period of FESC training effectively improves activity endurance in persons with chronic stroke8,17 or chronic SCI12,21,20. Mechanisms for improved activity endurance after a period of endurance training may include increased blood flow, increased capillary to fiber ratio, increased citrate synthase activity, improved oxidative and glycolytic enzyme activity; and/or transformation of fast glycolytic, fatigable muscle fibers to fast oxidative, fatigue resistant muscle fibers (i.e., type IIb/IIx to IIa).21
When it comes to persons with chronic stroke, two studies have addressed changes in activity endurance with use of FESC. In a prospective case series study by Alon et al, an increase in cycling endurance was reported after 8 weeks of FES/M-IC training performed 3 days per week for 30 minutes per session, as indicated by a 246% mean increase in cycling workload.8 However, a limitation of this study is that there was no control group to compare results with that either performed time matched nonassisted cycling or some other endurance activity. In a randomized-controlled trial (RCT) by Janssen et al, a statistically significant increase in walking endurance was reported after 8 weeks of FES-AC training, that produced continuous muscle overload, performed 3 days per week for 30 minutes per session, as indicated by a 14.5% mean increase in distance walked on 6-Minute Walk Test (6MWT). These investigators also include a time matched nonassisted cycling training group and reported statistically similar results between groups.17
When it comes to persons with chronic SCI, three studies have addressed changes in activity endurance with use of FESC. In a prospective case series study by Griffin et al12, a statistically significant increase in FES-IC endurance was reported after 8 weeks of FES-IC training performed 2-3 days per week for a target of 30 minutes per session (depending on tolerance), as indicated by a mean increase in cycling workload (presented graphically in the publication), in a group of persons with chronic incomplete or complete SCI. In a prospective case series study by Duffell et al21 that involved persons with complete SCI, a statistically significant increase in quadriceps endurance was reported after 3 months of FES-IC training performed 3-5 days per week for a target of 60 minutes per session (depending on tolerance). Increased quadriceps endurance was indicated by a mean decrease in quadriceps force loss of 28.3% after 3 minutes of NMES-induced quadriceps contraction at a current frequency of 40 Hz and pulse duration of 250 μs. Quadriceps endurance continued to increase for up to 9 months post intervention onset, as indicated by mean decreases in quadriceps force loss of 39% and 46.7% from baseline to 6 and 9 months, respectively. Lastly, in a prospective case report study by Donaldson et al that involved an individual with chronic incomplete SCI, an increase in cycling endurance was reported after 5 and 15 months of FES-AC training, as indicated by an increase in cycling distance performed in one bout of 733% and 900%, respectively, from baseline. However, a limitation of this study is that there was no control to compare results with that either performed time matched nonassisted cycling or some other endurance activity.
LE Spastic Muscle Tone
A period of FESC training effectively reduces spastic muscle tone in persons with subchronic14,15 or chronic18 stroke, or chronic complete SCI22. A neuromuscular hypothesis for the reduction in spastic muscle tone with cycling training is that it applies repetitive, reciprocal stretching that affects local neural pathways.26,27 A cardiovascular hypothesis for the reduction in spastic muscle tone with cycling training is that the added active muscle contraction improves local blood circulation that acts to reduce the actual mechanical stiffness of the viscous and elastic components of the muscle.28,29 Neurophysiological hypotheses for the enhanced reduction in spastic muscle tone with FESC training include: the reciprocal inhibitory affect on agonist muscles caused by stimulating the antagonist muscles30, but some researchers have demonstrated no significant changes when testing this mechanism31; the autogenic inhibitory affect on agonist muscles caused by stimulating the agonist muscles, however, no study evaluating long-term effects exists to my knowledge using this intervention; and the sensory habituating effect on the neural pathways beyond the stimulated area32,33 (e.g., reorganization of higher brain centers that initiate neuromuscular activity14).
When it comes to persons with subchronic stroke, two studies have addressed changes in spastic muscle tone with use of FESC. In a cross-sectional study by Yeh et al14, a statistically significant decrease in spastic muscle tone was reported after a 20 minute session of FES-AC, which was 80% greater than the decrease observed after 20 minutes of nonassisted cycling (p < 0.05), as measured by the modified Ashworth scale (MAS). In a cross-sectional study by Lo et al15, a statistically significant decrease in spastic muscle tone was reported after a 200 m trial of FES-AC, which was significantly greater than the decrease observed after a 200 m trial of nonassisted cycling, as measured by MAS.
In a RCT by Lo et al18 with persons affected by chronic stroke, a statistically significant decrease in spastic muscle tone was reported after a 20 minute session of FES-AC, which was significantly greater than the decrease observed in a control group after a 20 minute session of nonassisted cycling, as measured by MAS.
In a cross-sectional study by Krause et al22 with persons affected by chronic complete SCI, a statistically significant decrease in spastic muscle tone was reported after an FES-IC session, which was significantly greater than the decrease observed after a cadence and time matched session of passive motor-IC, as measured by MAS.
Limited Overground Walking Ability
A period of FESC training effectively improves overground walking ability in ambulatory individuals with subchronic9 or chronic8 stroke, and possibly in ambulatory individuals with chronic incomplete SCI.20 Mechanisms of improved overground gait speed after a period of FESC training include: improved muscle strength of bilateral LEs8,13; improved motor control of the paretic LE(s)8,13, improved coordination between bilateral LEs9,13; partial reversal of general deconditioning8; and/or improved trunk control9.
In a RCT by Ambrosini et al9 with persons affected by subchronic stroke, a statistically significant 255% mean increase in overground gait speed was reported after a 4 week rehabilitation program performed 5 days per week for 3 hours per day that included 25 minutes of FES/M-IC per session, which was insignificantly greater than the 164% increase in overground gait speed reported in the control group who performed passive M-IC in place of FES/M-IC.
In a case series study by Alon et al8 with persons affected by chronic stroke, a statistically significant 25% mean increase in overground gait speed was reported after 8 weeks of FES/M-AC performed 3 days per wk for 30 minutes per session. However, a limitation of this study is that there was no control to compare results with that either performed time matched nonassisted cycling training or some other training methods.
In a case study by Donaldson et al20, a single individual with chronic incomplete SCI was reported to have improved his functional ambulation ability after 16 months of FES-AC training performed for an average of 21 minutes per day. However, this is an extremely underpowered report that needs to be investigated further using a more highly powered study design.
Glucose Intolerance
In a prospective case series study by Griffin et al12 with persons affected by chronic incomplete or complete SCI, a statistically significant improvement in glucose tolerance (presented graphically in the publication) was reported after 8 weeks of FES-IC training performed 2-3 days per week for a target of 30 minutes per session, as determined by fasting glucose tolerance testing.
Mechanisms of improved glucose tolerance and insulin action after a period of FES-IC training may include: increased lean body mass, and therefore increased surface area for the intake of glucose; increased expression of glucose transporter type 4 (GLUT4) proteins in response to glucose exposure; increased enzymes that control intracellular glucose disposal; and/or increased influence of slow and fast oxidative muscle fibers (i.e., type I and IIa), which results in uptake of more glucose.12
Elevated Biochemical Inflammatory Markers Associated with Heart Disease
In a prospective case series study by Griffin et al12 with persons affected by chronic incomplete or complete SCI, a statistically significant decrease in biochemical inflammatory markers associated with heart disease was reported after 8 weeks of FES-IC training performed 2-3 days per week for a target of 30 minutes per session, as indicated by statistically significant 18.7%, 22.8% and 4.3% mean decreases in C-reactive protein, Interleukin-6 and tumor necrosis factor-α concentrations, respectively.
A hypothesized mechanism of reduction in biochemical inflammatory markers after a period of FESC is that this method of physical activity, like other methods of physical activity, results in reductions of several cardiovascular risk factors, such as BMI, waist hip ratio and the lipid profile, which are associated with increased inflammation in the body.35
References
- Centers for Disease Control and Prevention (CDC). (2011, December 07). About stroke. Retrieved from http://www.cdc.gov/stroke/about.htm
- National Stroke Association. (2013). STARS – Steps Against Recurrent Stroke. Retrieved on March 31, 2013 from: http://www.stroke.org/site/PageServer?pagename=stars
- New, P. W. & McFarlane, C. L. (2013). Survival following spinal cord infarction. Spinal cord, doi: 10.1038/sc.2013.14.
- National Spinal Cord Injury Association. (2011). Health & wellness after SCI. Retrieved on March 31, 2013 from: http://www.spinalcord.org/resource-center/askus/index.php?pg=kb.book&id=8.
- Roger, V. L., Go, A. S., Lloyd-Jones, D. M., Benjamin, E. J., Berry, J. D., Borden, W. B., et al. (2012). Heart disease and stroke statistics: A report from the American heart association. Circulation, 125(1), e2–220.
- Cardenas, D. D., Hoffman, J. M., Kirshblum, S., & McKinley, W. (2004). Etiology and incidence of rehospitalization after traumatic spinal cord injury: A multicenter analysis. Archives of physical medicine and rehablitions, 85(11), 1757-63.
- McKinley, W. O., Jackson, A. B., Cardenas, D. D., DeVivo, M. J. (1999). Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Archives of physical medicine and rehabilitation, 80(11), 1402-10.
- Alon, G., Conroy, V. M., & Donner, T. W. (2011). Intensive training of subjects with chronic hemiparesis on a motorized cycle combined with functional electrical stimulation (FES): A feasibility and safety study. Physiotherapy research international, 16, 81-91.
- Ambrosini, E., Ferrante, S., Pedrocchi, A., Ferrigno, G., & Molteni, F. (2011). Cycling induced by electrical stimulation improves motor recovery in postacute hemiparetic patients: A randomized controlled trial. Stroke, 42(4), 1068-73.
- Restorative Therapies. RT300-SL rehabilitation therapy. Retrieved on February 15, 2013 from: http://restorative-therapies.com/sage.
- Lai CH, Chang WH, Chan WP, Peng CW, Shen LK, Chen JJ, Chen SC. (2010). Effects of functional electrical stimulation cycling exercise on bone mineral density loss in the early stages of spinal cord injury. Journal of rehabilitation medicine, 42(2), 150-4.
- Griffin, L., Decker, M. J., Hwang, J. Y., Wang, B., Kitchen, K., Ding, Z., & Ivy, J. L. (2009). Functional electrical stimulation cycling improves body composition, metabolic and neural factors in persons with spinal cord injury. Journal of electromyography and kinesiology, 19(4), 614-22.
- Ferrante, S., Pedrocchi, A., Ferrigno, G., & Molteni, F. (2007). Cycling induced by functional electrical stimulation improves the muscular strength and the motor control of individuals with post-acute stroke. European Journal of Physical and Rehabilitation Medicine, 44(2), 159-67.
- Yeh, C., Tsai, K., Su, F., & Lo, H. (2010). Effect of a bout of leg cycling with electrical stimulation on reduction of hypertonia in patients with stroke. Archives of Physical Medicine and Rehabilitation, 91, 1731-6.
- Lo, H., Tsai, K., Su, F., Chang, G., & Yeh, C. (2009). Effects of a functional electrical stimulation-assisted leg-cycling wheelchair on reducing spasticity of patients after stroke. Journal of rehabilitation medicine, 41, 242-246.
- Szecsi, J., Krewer, C., Müller, F., & Straube, A. (2008). Functional electrical stimulation assisted cycling of patients with subacute stroke: Kinetic and kinematic analysis. Clinical Biomechanics, 23, 1086-1094.
- Janssen, T. W., Beltman, J. M., Elich, P., Koppe, P. A., Konijnenbelt, H., de Haan, A., & Gerritis, K. H. (2008). Effects of electric stimulation-assisted cycling training in people with chronic stroke. Archives of Physical Medicine and Rehabilitation, 89(3), 463-9.
- Lo, H. C., Hsu, Y. C., Hsueh, Y. H., & Yeh, C. Y. (2012). Cycling exercise with functional electrical stimulation improves postural control in stroke patients. Gait Posture, 35(3), 506-10.
- Liu, C. W., Chen, S. C., Chen, C. H., Chen, T. W., Chen, J. J., Lin, C. S., & Huang, M. H. (2007). Effects of functional electrical stimulation on peak torque and body composition in patients with incomplete spinal cord injury. The Kaohsiung journal of medical sciences, 23(5), 232-40.
- Donaldson, N., Perkins, T. A., Fitzwater, R., Wood, D. E., & Middleton, F. (2000). FES cycling may promote recovery of leg function after incomplete spinal cord injury. Spinal cord, 38(11), 680-2.
- Duffell, L. D., Donaldson, N., Perkins, T. A., Rushton, D. N., Hunt, K. J., Kakebeeke, T. H., &Newham, D. J. (2008). Long-term intensive electrically stimulated cycling by spinal cord-injured people: Effect on muscle properties and their relation to power output. Muscle & nerve, 38(4), 1304-11.
- Krause, P., Szecsi, J., & Straube, A. (2008). Changes in spastic muscle tone increase in patients with spinal cord injury using functional electrical stimulation and passive leg movements. Clinical rehabilitation, 22(7), 627-34.
- Hakansson, N. A. & Hull, M. L. (2010). The effects of stimulating lower leg muscles on the mechanical work and metabolic response in functional electrically stimulated pedaling. IEEE transactions on neural systems and rehabilitation engineering, 18(5), 498-504.
- Restorative Therapies. Over the phone price quote for the RT300-SL functional electrical stimulation and motorized leg cycle ergometer. Retrieved on March 08, 2013 from Restorative Therapies sales department at 1-800-609-9166.
- Gabriel, D. A., Kamen, G., & Frost, G. (2006). Neural adaptations to resistive exercise: mechanisms and recommendations for training practices. Sports medicine, 36(2), 133-49.
- Gajdosik, R. L. (2001). Passive extensibility of skeletal muscle: Review of the literature with clinical implications. Clinical biomechanics, 16(2), 87-101.
- Kubo, K., Kanehisa, H., Fukunaga, T. (2002). Effect of stretching training on the viscoelastic properties of human tendon structures in vivo. Journal of applied physiology, 92(2), 595-601.
- Evetovich, T. K., Nauman, N. J., Conley, D. S., & Todd, J. B. (2003). Effect of static stretching of the biceps brachii on torque, electromyography, and mechanomyography during concentric isokinetic muscle actions. Journal of strength and conditioning research, 17(3), 484-8.
- van der Salm A, Veltink PH, Ijzerman MJ, Groothuis-Oudshoorn KC, Nene AV, Hermens HJ. (2006). Comparison of electric stimulation methods for reduction of triceps surae spasticity in spinal cord injury. Archives of physical medicine and rehabilitation, 87(2), 222-8.
- Franek A, Turczynski B, Opara J. (1988). Treatment of spinal spasticity by electrical stimulation. Journal of biomedical engineering, 10(3), 266-70.
- Okuma, Y., Mizuno, Y., & Lee, R. G. (2002). Reciprocal Ia inhibition in patients with asymmetric spinal spasticity. Clinical neurophysiology, 113(2), 292-7.
- Wang, R. Y., Tsai, M. W., Chan, R.C. (1998). Effects of surface spinal cord stimulation on spasticity and quantitative assessment of muscle tone in hemiplegic patients. American journal of physical medicine & rehabilitation, 77(4), 282-7.
- Wang, R. Y., Chan, R. C., & Tsai, M. W. (2000). Effects of thoraco-lumbar electric sensory stimulation on knee extensor spasticity of persons who survived cerebrovascular accident (CVA). Journal of rehabilitation research and development, 37(1), 73-9.
- Verdaet, D., Dendale, P., De Bacquer, D., Delanghe, J., Block, P., De Backer, G. (2004). Association between leisure time physical activity and markers of chronic inflammation related to coronary heart disease. Atherosclerosis, 176(2), 303-10.
- Yan, T., Hui-Chan, C. W., & Li, L. S. (2005). Functional electrical stimulation improves motor recovery of the lower extremity and walking ability of subjects with first acute stroke: a randomized placebo-controlled trial. Stroke, 36(1), 80-5.
- Yeh, C., Tsai, K., Su, F., & Lo, H. (2010). Effect of a bout of leg cycling with electrical stimulation on reduction of hypertonia in patients with stroke. Archives of Physical Medicine and Rehabilitation, 91, 1731-6.


2 Responses to “LE Functional Electrical Stimulation Cycling for Stroke and SCI”
blindqui
Kyle,
Thanks for the great questions? Hopefully, I address them to your satisfaction. When it comes to provisional requirements for building and using an FESC system, it would come along with much more accountability than a commercially purchased FESC that comes with standby technical support from the company it was purchased from. You would need to ensure your systems safety and accuracy, which would most likely require a complex understanding of machine mechanics and electronics, execution of complex calibrations with built in fail-safes, and testing by a qualified agency to evaluate its safety and accuracy, which would need to be completed periodically even after initial evaluation.
When it comes to reimbursement, you may have misread the information I provided. Medicare actually DOES pay for FESC and the process of reimbursement is outlined in my presentation.
When it comes to the referenced evidence, being largely case-control studies in the population of the SCI. This is due to the fact that there is not much else available to compare FESC with that enables these patients to use their own muscles to perform the exercise in question. Most of the benefits researched for this population are cardiovascular in nature, which can be accomplished through upper body ergometer training if the person in question does not have upper extremity involvement, but only to a limited degree that does not necessarily impact health of the lower extremity vasculature and anatomy. Additionally, systems are available that come with an upper body ergometer, which can also be synchronized with FES. The studies investigating changes in spasticity were largely cross-sectional in design, which was appropriate for the clinical question. The information from these studies reflect that FESC is effective, and more effective than passive/motor-induced cycling. However, it does not necessarily mean that FESC is better than an intervention like PNF. Keep in mind though that this is simply another tool that can be used with these populations.
This brings me to your question about a comparison between BWSTT and FESC. This is also a case where one is not necessarily better than the other, but merely different tools in your toolbox. However, depending on the point in recovery, some patients may not be able to volitionally perform steps or may have some other comorbidity that makes a standing position too difficult or not tolerable, so really it depends on patient characteristics on which of the two interventions would be more appropriate given a limited amount of time for therapy.
For your final question, just like anything else the cost needs to be weighed against the benefits, which will vary depending on the target of a practice. If you own a clinic that specialized in rehabilitation post SCI, an FESC would likely be a good investment. However, when it comes to stroke, this may be less clear, but would still need to be considered on a case-by-case basis, based on the proportion of patients that could benefit from the intervention and the level of concern for the therapists that are employed in the practice and if they are at risk of injury by providing straining gait training efforts to certain patients.
-Brandon
Kyle Hoppes
Hey Brandon,
Thank you for your extensive review of FESC in patients with either stroke or SCI. I have just a few questions that I am wondering if you came across in your research:
What provisional requirements are necessary for someone to create his or her own system?
If Medicare isn’t paying for FESC, then are other insurances paying for it? What would be the cost for a patient without an insurance that covers it?
In reviewing your summary of the literature I noticed that many of the studies did not include control groups. To me this makes it difficult to compare and contrast various protocols. How do you believe the use of FESC compares to BWSTT in patients post-stroke? If you had to recommend either FESC or BWSTT to a rehabilitation unit which would it be, and why?
I also was wondering what your final conclusion was or what you took away from all the information? You present several studies that show improvements but when you weigh in cost, reimbursement, and time, does it make sense to transition the equipment into the clinic?
Thanks,
Kyle