IMMEDIATE EFFECTS OF A STANCE CONTROL KNEE-ANKLE-FOOT ORTHOSIS ON GAIT IN PEOPLE WITH SUBACUTE STROKE
David D Morse, SPT UNC Chapel Hill; Gabrielle Scronce, PT, DPT; Vicki S Mercer PT, PhD.
University of North Carolina at Chapel Hill
How this Project Began
Prior to and during my time as a DPT student at UNC I took part in a research project with Dr. Vicki Mercer and Dr. Gabrielle Scronce. I was present early on during the project and was included in discussions with UNC Hospitals Inpatient Rehab concerning the logistics of patient recruitment and testing in their facility. I also assisted in grant writing, which eventually resulted in funding through LSVT Big. Once the study began in earnest, I assisted in patient screening and testing, as well as SCKAFO fitting and training. I performed a large part of the data collection and data processing using GAITRite. Subsequently, I created and presented a poster at the NCPTA Conference with 8 subject’s data during my first year as a DPT student. This work formed a solid base on which to build a capstone project. I chose to statistically analyze and present the results of our continued recruitment of subjects through the 2019 Spring semester resulting in a total of 13 patients with over 50 patients screened as a whole. This included creation and presentation of a poster and updated statistical analysis as presented bellow.
Introduction and Purpose
Improving walking ability is an essential goal for individuals with hemiparesis after stroke. Current evidence stresses the need for high doses of stepping practice during rehabilitation to improve walking ability, but early practice is often limited by weakness and instability of the paretic lower extremity (LE). Use of a training stance control knee-ankle-foot orthosis (SCKAFO) may provide the support necessary for increased walking practice in the early post-stroke period. The purpose of this study was to obtain preliminary evidence regarding immediate effects and user perspectives from individuals with recent stroke walking with and without a training SCKAFO.
Literature Review
Improvement of walking ability is a primary goal for people with hemiparesis after stroke.1, 2 Although most stroke survivors regain the ability to walk,3 their gait is often slow, asymmetrical, and energy-inefficient.4-7 Almost one third of people living at home after stroke are unable to walk unsupervised in their communities.2 Clearly, additional research is needed to determine the best approaches for maximizing walking recovery after stroke.
Recent evidence suggests that task-specific training8-1o and higher intensity of practice via high repetition11 may be essential elements for optimal walking recovery. Task-specific training, also referred to as task-oriented or task-related training, is any intervention in which the activity that is the target of the intervention is practiced using a functional approach.12 When the focus is on improving walking ability, task-specific training typically includes overground walking-related tasks or treadmill training with or without body-weight support.10, 12 Strong evidence indicates that, regardless of the task, more practice is better.11 Gait training, which involves a high number of repetitions executed within a single treatment session, provides the repetitive task practice that is critical after stroke.13, 14
These two motor learning principles, specificity of training and repetition, are thought to promote activity-dependent plasticity of the central nervous system during stroke recovery.15 After damage to the motor cortex, rehabilitative training can shape reorganization in adjacent undamaged cortical areas.16 This reorganization reflects true recovery, in that the intact brain regions generate commands to the same muscles that were used to perform the task prior to the stroke. In contrast, compensation involves the use of alternative muscles to achieve the task goal.16 True recovery may be maximized by providing appropriate training within the first three to four weeks post stroke, when the potential for neuroplasticity is greatest.11
Individuals with significant hemiparesis following a stroke often require assistance for walking, especially in the first few weeks of recovery. Alternatives for task-specific, repetitive training include partial body weight supported treadmill training (BWSTT), functional electrical stimulation (FES), robotic training (e.g., using the Lokomat), and bracing using a knee-ankle-foot orthosis (KAFO) or ankle-foot orthosis (AFO).15, 17 Results of studies of BWSTT have been mixed, and this intervention can be impractical, as the patient may need manual assistance for gait mechanics (e.g., for knee joint stability in weight bearing on the paretic limb or to advance the paretic limb during the swing phase of gait). Such manual assistance can be overly burdensome for rehabilitation specialists.15 Likewise, multichannel surface FES systems are impractical because of the time required for donning, nonspecific muscle activation, and lack of portability.15 Use of intramuscular electrodes for FES is invasive, carrying a risk of infection and other complications, and requiring specialized expertise that is not widely available. Both BWSTT and robotic training require expensive equipment that typically is not portable.
Bracing with a KAFO within two to four weeks after stroke has been shown to increase endurance and speed of ambulation.17 A major drawback of conventional locked-knee KAFOs is that they produce compensatory movements such as hip elevation or circumduction for foot clearance during the swing phase of gait. Recently developed stance-control KAFOs (SCKAFOs), on the other hand, stabilize the knee in stance and automatically release in swing, permitting normal gait mechanics.18, 19 During swing phase on the paretic side, SCKAFOs provide functional shortening of the paretic lower limb for ground clearance while at the same time converting the limb to a compound pendulum, enabling the leg to swing forward with less effort18 SCKAFOs have been shown to improve velocity, symmetry, and other spatiotemporal characteristics of gait when compared to walking with conventional locked-knee KAFOs in various patient populations20-22 and when compared to walking without orthoses in individuals with chronic hemiparesis after stroke.19 The use of SCKAFOs for patients undergoing inpatient rehabilitation following stroke has not been reported previously in the literature.
The purpose of the proposed study was to determine the feasibility and obtain preliminary evidence concerning the effectiveness of early gait training with SCKAFOs in individuals recovering from stroke. This intervention applied the motor learning principles of specificity of training and repetition. We expected that the use of training SCKAFOs would enable people post-stroke who have significant weakness of the affected lower limb to begin walking practice earlier and with greater intensity than would be possible without the SCKAFO. This intense walking practice, in turn, was expected to promote neuroplasticity for normal amplitude and timing of muscle activation, resulting in a smoother, more symmetrical gait pattern without compensations.
Methods
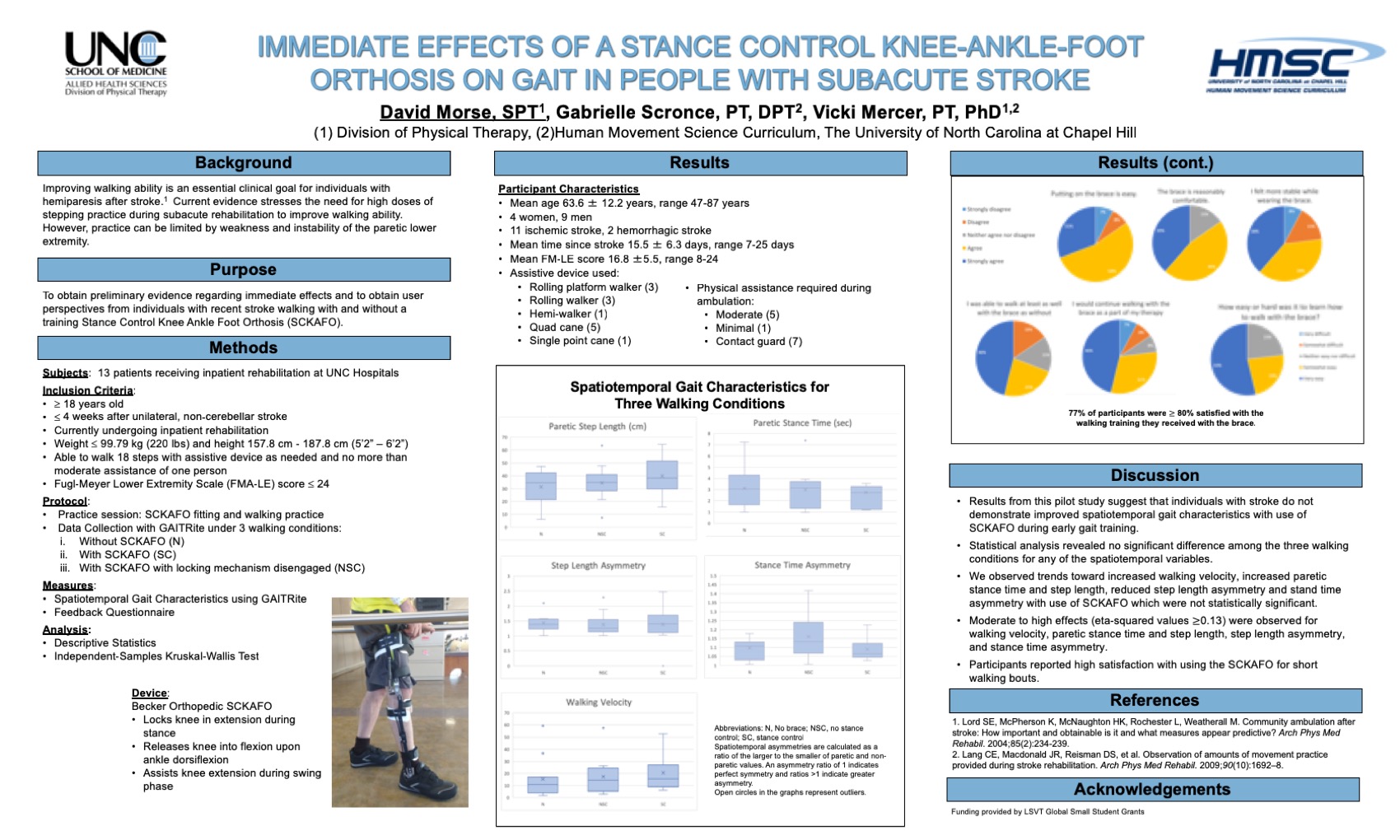
Thirteen patients receiving inpatient rehabilitation at UNC Hospitals were enrolled in this study. Key eligibility criteria included recent stroke causing significant unilateral LE weakness as indicated by a Fugl-Meyer LE motor scale score £ 24, currently undergoing inpatient rehabilitation, and able to walk 18 steps with no more than moderate assistance of one person. Participants’ gait speed, step length asymmetries, and stance time asymmetries were collected using a GAITRite instrumented walkway during short walks under 3 conditions: 1) without SCKAFO, 2) with non-functioning SCKAFO (mechanism disengaged), and 3) with SCKAFO functioning as intended. A follow-up questionnaire was administered to elicit participants’ perspectives of walking with and without the SCKAFO. Descriptive statistics were used to characterize the performance of the study participants under the 3 walking conditions and to summarize feedback about the orthosis. Due to small sample size and large variability within groups, a non-parametric measure of differences between our 3 groups (Independent-Samples Kruskal-Wallis Test) was used.
Results
Walking with the SCKAFO resulted in significantly faster gait speed (0.208 ± 0.014 m/s) compared to walking without the SCKAFO (mean 0.148 ± 0.162 m/s; p = 0.03). Non-significant improvement in step length symmetry and no change in stance time symmetry occurred when participants walked with the SCKAFO compared to without. Participants reported an average of 9 ± 1.4on a 10-point scale of overall satisfaction with walking training with the SCKAFO for short periods within this study. Ten (76.9%) participants reported that they agreed or strongly agreed with the statement, “If given the option, I would like to continue walking training with the brace as part of my physical therapy.”
Conclusions
Participants performed short bouts of walking with significantly improved gait speed and trends toward increased spatial symmetry between paretic and non-paretic LEs when walking with compared to without a SCKAFO. This included reduction in step length and stance time asymmetry values. Moderate to high effects (eta-squared values ≥0.13) were observed for walking velocity (0.25), paretic step length (0.279), step length asymmetry (0.278), and stance time asymmetry (0.13). Increase in paretic step length could have contributed to increased walking velocity when wearing the SCKAFO. Also, participants reported feeling much more stable when wearing the SCKAFO potentially contributing to the increased stance time on the paretic limb. All of the subjects were taking shorter steps with their paretic leg when compared to their non-paretic side. Consistent increases in step length when wearing the brace contributed to reduced asymmetry when walking with the SCKAFO. Increased time spent on the paretic leg when wearing the SCKAFO contributed to the reduction in stance time asymmetry.
Participants reported high satisfaction with using the SCKAFO for short walking bouts. Greater than 85% of participants also reported that the brace was easy to put on and take off and was comfortable. Greater than 75% of participants felt more stable with the brace than without, would continue walking with the brace, and felt they could walking at least as well with the brace as without. Seventy-seven percent of participants though it at least somewhat easy to learn how to walk with the brace.
Adjustment of the brace was done completely by the research team often requiring two individuals. Two individuals (one clinician and one student) were also needed during walking training and adjustment of the dorsiflexion release mechanism at the knee. Further, the brace occupied extra space on the medial and lateral sides of the ankle requiring a shoe with a flexible or roomy heel cup which did not rise up past the ankle joint of the brace or interact with the tensioning cables connecting the ankle joint to the dorsiflexion release levers a the knee. The cast shoes used in this study were problematic in that the back of the shoe would compress the tensioning cables, affecting the ability of the brace to lock in knee extension. Fitting and adjustment of the brace required specialized knowledge and skill and could prove a barrier to PT utilization in the inpatient rehabilitation setting. Further investigation and analysis are needed to determine the effects of using a SCKAFO more regularly during rehabilitation from recent stroke.
References
- Bohannon RW, Andrews AW, Smith MB. Rehabilitation goals of patients with hemiplegia. Int J Rehabil Res. 1988;11:181-183.
- Lord SE, McPherson K, McNaughton HK, Rochester L, Weatherall M. Community ambulation after stroke: how important and obtainable is it and what measures appear predictive? Arch Phys Med Rehabil. 2004;85:234-239.
- Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS. Recovery of walking function in stroke patients: the Copenhagen Stroke Study. Arch Phys Med Rehabil. 1995;76:27-32.
- Wade DT, Wood VA, Heller A, Maggs J, Langton Hewer R. Walking after stroke. Measurement and recovery over the first 3 months. Scand J Rehabil Med. 1987;19:25-30.
- Wall JC, Turnbull GI. Gait asymmetries in residual hemiplegia. Arch Phys Med Rehabil. 1986;67:550-553.
- Hill KD, Goldie PA, Baker PA, Greenwood KM. Retest reliability of the temporal and distance characteristics of hemiplegic gait using a footswitch system. Arch Phys Med Rehabil. 1994;75:577-583.
- Olney SJ, Monga TN, Costigan PA. Mechanical energy of walking of stroke patients. Arch Phys Med Rehabil. 1986;67:92-98.
- Hornby TG, Straube DS, Kinnaird CR, et al. Importance of specificity, amount, and intensity of locomotor training to improve ambulatory function in patients poststroke. Top Stroke Rehabil. 2011;18:293-307.
- Hornby TG, Holleran CL, Leddy AL, et al. Feasibility of Focused Stepping Practice During Inpatient Rehabilitation Poststroke and Potential Contributions to Mobility Outcomes. Neurorehabil Neural Repair. 2015.
- DePaul VG, Wishart LR, Richardson J, Thabane L, Ma J, Lee TD. Varied overground walking training versus body-weight-supported treadmill training in adults within 1 year of stroke: a randomized controlled trial. Neurorehabil Neural Repair. 2015;29:329-340.
- Veerbeek JM, van Wegen E, van Peppen R, et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS One. 2014;9:e87987.
- DePaul VG, Wishart LR, Richardson J, Lee TD, Thabane L. Varied overground walking-task practice versus body-weight-supported treadmill training in ambulatory adults within one year of stroke: a randomized controlled trial protocol. BMC Neurol. 2011;11:129-2377-11-129.
- French B, Thomas LH, Leathley MJ, et al. Repetitive task training for improving functional ability after stroke. Cochrane Database Syst Rev. 2007;(4):CD006073.
- Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol. 2009;8:741-754.
- Daly JJ, Ruff RL. Construction of efficacious gait and upper limb functional interventions based on brain plasticity evidence and model-based measures for stroke patients. ScientificWorldJournal. 2007;7:2031-2045.
- Krakauer JW. Motor learning: its relevance to stroke recovery and neurorehabilitation. Curr Opin Neurol. 2006;19:84-90.
- Kosak MC, Reding MJ. Comparison of partial body weight-supported treadmill gait training versus aggressive bracing assisted walking post stroke. Neurorehabil Neural Repair. 2000;14:13-19.
- Fatone S. A review of the literature pertaining to KAFOs and HKAFOs for ambulation. J Prosthet Orthot. 2006;18(7):137-168.
- Boudarham J, Zory R, Genet F, et al. Effects of a knee-ankle-foot orthosis on gait biomechanical characteristics of paretic and non-paretic limbs in hemiplegic patients with genu recurvatum. Clin Biomech (Bristol, Avon). 2013;28:73-78.
- McMillan AG, Kendrick K, Michael JW, Aronson J, Horton GW. Preliminary evidence for effectiveness of a stance control orthosis. J Prosthet Orthot. 2004;16:6-13.
- Yakimovich T, Lemaire ED, Kofman J. Gait evaluation of a new electromechanical stance-control knee-ankle-foot orthosis. Conf Proc IEEE Eng Med Biol Soc. 2006;1:5924-5927.
- Davis PC, Bach TM, Pereira DM. The effect of stance control orthoses on gait characteristics and energy expenditure in knee-ankle-foot orthosis users. Prosthet Orthot Int. 2010;34:206-215.
Link to high resolution poster images:
Box Plots
David Morse HMSC Poster 2019 box plots
Pie Charts
David Morse HMSC Poster 2019 pie charts
Acknowledgements
Thanks to Dr. Vicki Mercer and Dr. Gabrielle Scronce with whom I worked during the entirety of this project. I am so grateful that you were willing to bring me into the research project early on, even before I was in PT school. Thanks also to all the folks at UNC Inpatient Rehabilitation for their help in patient recruitment and use of your facilities.

4 Responses to “Immediate Effects of a Stance Control Knee-Ankle-Foot Orthosis on Gait in People with Subacute Stroke”
Debbie Thorpe
David
Really great work! Hope you will submit this for a poster at CSM next year. I agree with Vicki that you are PhD material!
Vicki Mercer
Great work on this project David! I hope that we can continue to work to identify those patients for whom this type of gait training will be most effective. Also hope to see you in a PhD program in a couple of years!!
Deborah Guthmann
David,
As always, your work is educational and of high-quality. I certainly learned more about gait rehabilitation from your capstone and ways in which to enhance my future practice. Your literature review succinctly walked me through the project’s purpose and importance as well as the reasoning behind the use of SCKAFO. I had not realized how impactful this orthosis could be on the stroke population. The preservation of normal gait mechanics through automatic release in swing has such huge potential for improving ambulation post-stroke! In my inpatient neuro rotation, I found that orthoses were often needed for stabilization but significantly impacted restoration of typical ambulation. The fact that subjects trended ‘toward increase spatial symmetry between paretic and non-paretic LEs’ is fantastic and definitely has implementations for the clinic. It was surprising that this hasn’t been trialed in the inpatient rehabilitation. I enjoyed reading through your methods, results and conclusions. It seems like you have excellent, preliminary evidence for use of this orthosis.
Your project seemed time consuming and thorough. It truly is amazing that you were able to put so much time and effort into research during your time at PT school—though I would expect nothing less from you! It also shows your commitment to both evidence and your future patients. While you incorporated research into your program, it was heavily grounded in practical utility for the betterment of your patients’ lives. I’m excited for you to carry that forward into your career. Once again, congratulations on the completion of an excellent project.
David Morse
Deb,
Thanks for taking the time to read through my Capstone!
This project gave me some good insight not only into the application of the SCKAFO in the inpatient rehabilitation setting but also the process of working with a hospital like UNC to investigate something potentially clinically useful. Frustrating at times and really fun at others I look forward to doing more research in the future. I am glad you found it informative and clinically meaningful!