Introduction:
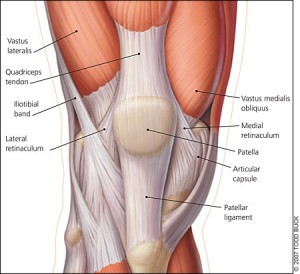
My DPT Capstone project focused on various areas to assess for patellofemoral pain syndrome, special tests to rule out competing diagnoses, and intervention ideas to rehabilitate these patients. Due to my interest in all settings of physical therapy thus far (I blame my excellent clinical instructors!), it took me quite some time to determine the focus of my Capstone. I landed on patellofemoral pain syndrome (PFPS) because I believe that in every setting, you will inevitably come across a patient with knee pain. When the pain begins with an insidious onset and includes specific activities/positions that influence the pain and function, where does one begin the evaluation?
The definitive etiology of PFPS is unknown, and it is often considered a multifactorial condition. There are many areas the clinician should assess when evaluating a patient with anterior knee pain. My upcoming clinical rotation is in an outpatient orthopedic setting with an emphasis on sports rehabilitation. I knew I would see multiple patients with knee pain in this population. I wanted to be fully prepared to effectively evaluate these patients and have a tool box of evidence-based interventions to use once I was able to determine the cause(s). In our Evidence Based Practice II class, I focused my research on the difference between hip and quadriceps strengthening to decrease pain and improve function in patients with PFPS. For my Capstone, I expanded this topic to include other intervention strategies as well as an efficient way to assess a patient with suspected PFPS.
Products:
During EBP II, I created an evidence table including articles describing hip and quadriceps strengthening for patients with PFPS as well as a literature review. [ Dean, D Module 4 ] [ Dean, D Module 5 ]. The evidence table was further developed with many of the articles I read for this presentation that supplemented the information I had previously gathered. This included articles on patellar taping and foot mechanics, as well as other topics I found pertinent to this diagnosis. [ Evidence table 1 ] [ Evidence table 2 ]
My weakness during clinical rotations has been the flow of an evaluation and I sought to create a product that would enable students and clinicians to have a well-organized process to follow. The assessment tool [ Assessment Tool – PFPS ] is intended as a basic format to follow in the clinic with subheadings of the patient’s position to make the evaluation more efficient. The first page is a check list with room to take notes and is meant for the clinician or student to bring with them when evaluating a patient with suspected patellofemoral pain. My hope is that this handout will provide an efficient and organized process in which to evaluate patients with anterior knee pain. The second and third pages include intervention strategies that may be used once the therapist has identified the suspected cause of the patellofemoral pain. While the assessment tool offers evidence-based suggestions, the program should certainly be individualized to each patient and will often include multiple components.
I provided a PowerPoint presentation to a group of DPT students (four 1st years and four 3rd years) along with 3 UNC faculty members on April 16, 2013. [ Patellofemoral Pain Syndrome – Capstone 2013 ] [ References ] Following the presentation, I received a feedback form from all participants regarding my ability to clearly present the information and what they felt they could take away from this presentation. [ Evaluation and Feedback form ] A brief summary is provided regarding scores and comments from the 11 participants in no particular order. [ Scores and Feedback ] From the feedback provided, I realized the information was a lot to process for the 1st year students who have not yet been educated on the knee. For future presentations, I plan to be even more aware of who my audience will be and ensure that I include more visuals for special tests that they may not be familiar with. Overall, this was an excellent experience for me and I hope I was able to further educate on the diagnosis of PFPS to the few students and faculty who were able to attend, as well as anyone who visits this site!
Special thanks:
To you for visiting my Capstone page! Also a huge thanks to Lori Von Alten, Mary Draize, and Mike Lewek who all helped me work through ideas and opened my eyes to different ways of thinking. A very, very (ten more very’s) big thanks to Mike Gross who helped me a considerable amount from the start to finish of this project, making himself available at any time to have discussions with me about my Capstone project.


8 Responses to “Patellofemoral Pain Syndrome: Assessment and Intervention Strategies”
Mike Gross
Donna- Excellent work on this entire project. I think it was a good learning experience for you, and the outcome products were very helpful resources to other folks. Mike Gross
Donna Dean
Thanks for your comments, Nick! It is certainly easy to get into the habit of assuming that one thing causes another as your CI did, but we MUST look at the whole person and determine exactly what is the cause…NEVER assume! I am sure you agree that our program has taught us that concept very well and this capstone project really drove that home for me.
Thanks again for checking it out!
Donna
Nick Camilleri
Donna,
You did such a great job on this project! You chose a really good topic; I saw so many cases of PFPS on my outpatient ortho rotation and had such a difficult time trying to figure out where to begin. My CI was convinced that weakness of the hip rotators was responsible for all PFPS, so I am glad that you have now given me the tools to help figure out and treat ALL of the contributing factors. I had the same question as Angela about time frames so thanks for already answering that!
Your powerpoint looks great and I wish I got to be there to see you present it. I particularly found the information about VMO:VL ratio and how we can affect this to be very useful. I was unaware that there was such a difference in activation between isotonic and isometric contractions so will definitely be utilizing that information in the future.
Great job!
Nick
Donna Dean
Alex – Thank you! I am so glad to be able to provide something that will help classmates in the future.
Joanne – From what I have read, orthotics and/or hip strengthening should be considered for “squinting” patella as the femoral antetorsion along with other factors may lead to pronation. Excessive hip IR and ADD may also be coming from weak hip musculature, causing this appearance of the patella. Anyone can correct me if I am wrong on this!
Lauren – You may absolutely have permission to give anyone access to my handout!
Angela – I read articles regarding different interventions that suggested a reduction in pain was made anywhere from 2-4 weeks after an intervention of some kind was implemented (whether it be an exercise program, taping, orthotics, or a combination of many things!). The main thing is to determine what is the cause of the pain, you can mask it and relieve the patient’s symptoms, but if you do not get to the root of the cause then it will certainly return (as we learned in Advanced Ortho). Modification of activities that influence the pain is important as well. If you are treating the patient while they’re continuing to run marathons on the weekend even through pain/discomfort, they might never have the pain resolved! If you can find the cause and decrease their symptoms, a gradual progression into more vigorous activity is key to be sure they are maintaining proper alignment and form.
Thanks for all of your comments!
Donna
alauten
Donna D!
I really wanted to comment on your Capstone because I was able to attend your presentation! You clearly demonstrated a thorough knowledge of the assessment and treatment of PFPS. And if I’m being honest, before your project, I had no clue what the best way was to go about diagnosing this issue. I really appreciate that in your assessment tool, you provide a comprehensive (yet simple) list of things to check that may contribute to PFPS, in addition to providing some nice options for intervention – also, thank you for referencing some of the articles for these, because I’m sure I might have to go back to the original articles at some point!
As I was looking over your materials again, I was wondering if you came across anything that gave a general time-frame for this kind of pain to resolve? Obviously, I know this is a HUGE “it depends” situation, with different patients have different causes/symptoms/severity, but in GENERAL, did you come across a time-frame for changes in pain or return to more vigorous activity?
Overall, I think you did a great job!! Thank you again for presenting on this rather mysterious and hard-to-diagnose condition!
lbsuggs
Donna,
Great job on this project! The information you provide is very comprehensive and the handout is such a great resource for students, including myself! Like Alex, I have already saved it for future use! This will be a perfect document to have on hand during clinical rotations, because as you know, there are many times when we don’t know where to start or in what order to proceed. The handout does a great job of systematically examining a patients with anterior knee pain. If I come across someone in the clinic who would benefit from your handout, may I have your permission to give them access?
What I like most about your project is that you stress the importance of an assessment that extends beyond the knee. This is key. If someone comes in with knee pain and we only look at the knee, then we are not being thorough and most likely not addressing the cause of the problem. Thank you for reminding us to extend our focus beyond the knee to the lumbopelvic region, the hip, and the foot/ankle.
ljoanne
Donna,
Great project! This is a condition I have often wondered about and not known where to begin with my evaluation. As I can see from your powerpoint and assessment tool, there are a large number of factors that can cause PFPS. I especially liked your assessment tool. This will be a very handy tool to keep with us in the clinic and I like the format you created so we can go down the list and check off everything as we assess them.
I’ve been also interested lately in taping and how that can impact the knee and shoulder. It was helpful to look over your evidence table and see specific articles that reference the use of taping for this diagnosis. I had one question, which you may of touched on at some point. During the assessment I saw that you included many tests to look at the position and extensibility of the soft tissues around the joint and you mentioned one thing to look for was squinting patellae from excessive femoral antetorsion. Did you find treatments to assist in correcting this cause of the pain? Just wondering since I know we have learned that knee pain can be caused from foot or hip biomechanics, if there was any interventions to assist with this source of pain.
Thanks again for all of your resources and everything looks great!
Alexandra Smith
Hi Donna,
Thanks for the great information on patellofemoral pain syndrome (PFPS). I really enjoyed reading over all of your information and I am so bummed that I missed your presentation. Judging by the results of your evaluation and feedback form it sounds like it was a great presentation!
Many patients that we see will come in with insidious knee pain, so I am so glad that I have your paper, PowerPoint presentation, and assessment toolbox as clinical resources. I have actually already printed out your assessment toolbox and I am sure that I will use it in the near future!
Thanks and GREAT JOB!