The Effects of Lower Extremity Strength on Verbal Cueing Response in Gait Rehabilitation Post-Stroke
_______________________________________________________________________
By Ben Buchanan
PRELUDE
_______________________________________________________________________
In my second clinical rotation of PT school I was introduced to the Inpatient Rehab setting, where I was exposed to a variety of individuals who had survived both traumatic brain injury (TBI) and stroke. I found it intriguing that subtle differences between areas affected within the brain could have vast disparity in the characteristics of its expression. While working with my clinical instructor, occupational therapists and speech language pathologists, I found that there were a great repertoire of tools or tricks one could use to provoke different responses for treatment depending on the type of presentation. This prompted me to learn more about how our behaviors, as physical therapists, no matter how subtle, influences our patients post-stroke. In my fall semester of my third year of PT school I had the opportunity to participate in a research experience with Dr. Michael Lewek, PT, PhD, working directly with patients’ post- stroke. The purpose of our study was to determine whether individuals with hemiparesis following stroke could experience functional gait changes with verbal cueing and whether residual strength in these individuals played a significant role in contributing to these changes.
ACKNOWLEDGEMENTS
_______________________________________________________________________
The materialization of this research would not have been possible without the relentless and determined help of Dr. Michael Lewek, PT, PhD who not only inspired me to continue this research, but also trusting me to provide best practice independently in a research setting. Furthermore, the research and preparation of this project would not be possible without my trusted colleague, classmate, and research partner, Hailey Guerin, SPT, who contributed a great deal of time, effort and insight into how to make this project what it is. I would also like to thank my committee members, Vicki Mercer, PT, PhD, and Jon Hacke, PT, OCS for their valuable feedback and guidance along the way. To all of the faculty in the UNC DPT program for instilling within me the pursuit of evidence-based practice in the clinical setting for the betterment of all, and finally to my clinical instructor Sharon Wong, PT, DPT, ATC for inspiring me to pursue this interest during my clinical rotation.
ABSTRACT
_______________________________________________________________________
OBJECTIVE
Current rehabilitation for gait retraining post-stroke involves some degree of strength training as weakness is commonly observed in the affected extremity. There is limited evidence that strength training alone improves functional ambulation. The purpose of this study is to determine what effect lower extremity strength has on the amplitude of change in specific functional gait parameters when given specific spatiotemporal verbal cues during gait rehabilitation.
METHODS
Twenty-nine adults with unilateral hemiparesis and a history of chronic stroke were assessed for lower extremity muscle strength using a hand-held dynamometer measuring hip flexion, abduction, knee flexion, extension, and ankle plantar flexion, dorsiflexion. Gait assessment was then performed consisting of: (1) Comfortable gait speed (CGS); (2) Fast gait speed; (3) Walking with long steps; (4) Walking with high steps; (5) Walking with a focus on arm swing; (6) Walking with a focus on pushing off of the ground with each step; (7) Walking taking quick steps; and a final (8) Comfortable gait speed. The first and last cues were always CGS. During steps 2-7, verbal cueing was randomized for each subject. Gait parameters of: walking speed, step length, stance time, and cadence were recorded using a GAITRite mat in order to measure spatiotemporal changes. The relationships between each verbal cue and each gait parameter were then analyzed.
RESULTS
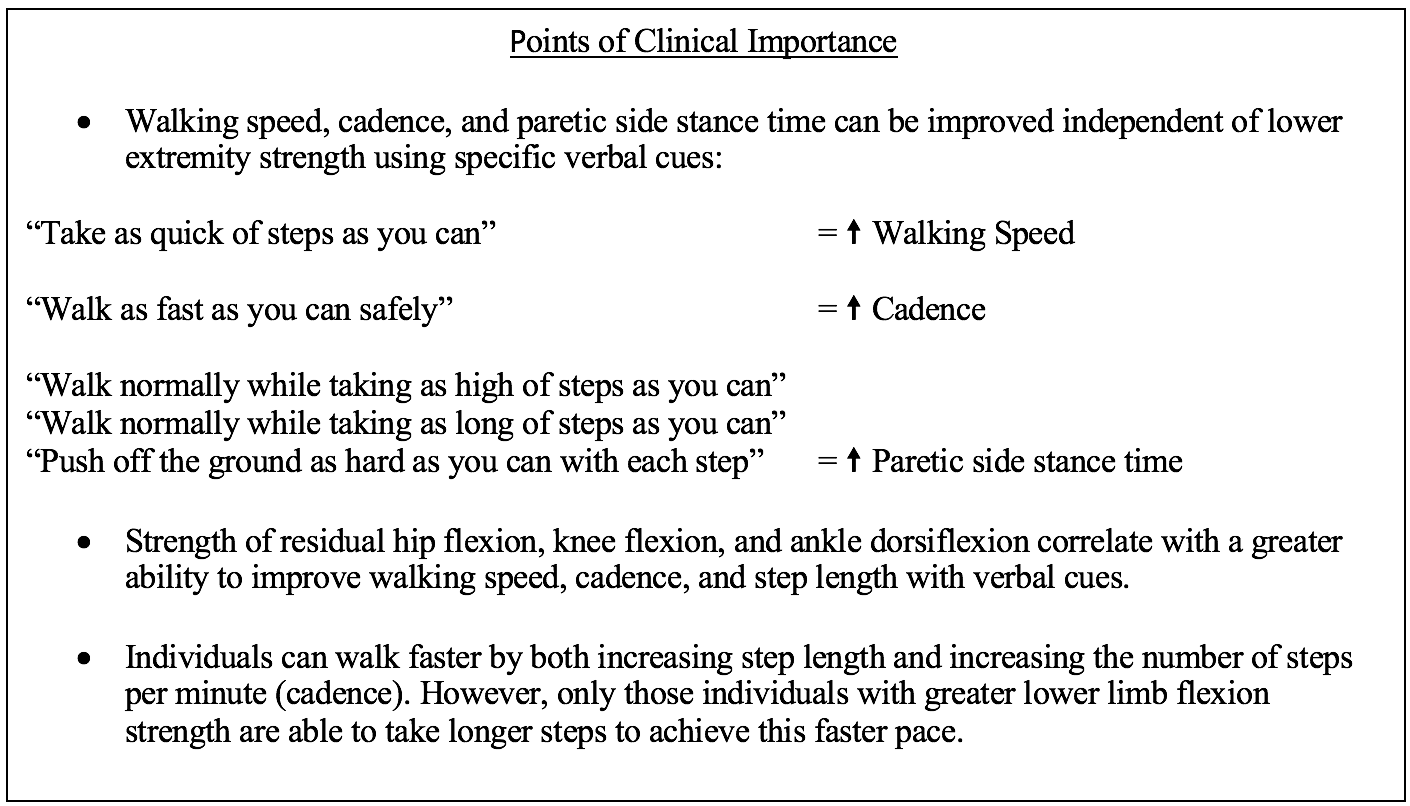
With specific verbal cues, subjects were able to significantly increase walking speed, cadence, and paretic side stance time independent of lower extremity strength. Individuals with residual hip flexion, knee flexion, and ankle dorsiflexion strength, subjects were able to elicit a significant response to walking speed, cadence, and step length with specific verbal cues.
CONCLUSION
By using specific verbal cueing, strength deficits in individuals with post-stroke hemiparesis can be circumvented to elicit significant changes in walking speed, cadence, and paretic side stance times. Similarly, the use of specific verbal cueing, can also be used to elicit significant changes in walking speed, cadence and step length in individuals with residual hip flexor, knee flexor and ankle dorsiflexor strength.
Introduction
_______________________________________________________________________
Stroke is the leading cause of long-term disability in the United States.1 Every year 795,000 individuals in the US experience a stroke and over half of all stroke survivors over the age of 65 experience negative effects on mobility.1 Falls and mobility-related injury are one of the most common complications post-stroke occurring in 25-30% of all stroke survivors.2 Falls can lead to further injury, increased risk of falls, increased hospitalization, increased cost, and decreased independence.3,4 Walking is the most common activity leading to falls in community-dwelling stroke survivors.4 Furthermore, walking is one of the most frequently self-selected goals for individuals in rehabilitation that necessitates a return to community ambulation and functional ADLs.5 Therefore, gait re-training is one of the most essential aspects of therapy post-stroke.6–8
There are a variety of factors involved in gait impairment. One primary factor is lower extremity hemiparesis, which impairs proper limb function during gait, such as the ability to bear weight, maintain stability, generate propulsion, and create swing of the affected lower extremity.9 In addition, stroke can create abnormalities in selective motor control, spasticity, and muscle atrophy leading to gait asymmetries, loss of balance, increased fear of falling, decreased gait speed and falls.10–14
In most individuals post-stroke, strength deficits eclipse joint mobility deficits limiting specific movements necessary for normal gait. Passive range of motion (PROM) in the lower extremity does not exhibit significant deficits,15 and may be less of a contributing factor than strength deficits in leading to overall gait impairments.15 Some of the common gait impairments observed following stroke include shortened step length, slower gait velocity, reduced cadence, reduced non-paretic swing times and reduced paretic stance times.16–18 Functional gait parameters have been shown to be heavily influenced by the degree of strength in the hip flexors, hip extensors, and hip abductors.19 Gait asymmetries, both spatial and temporal, are commonly attributed to decreased strength of the ankle plantar flexors and knee extensors.20,21 In addition, the total work produced by knee extension, ankle plantar flexion and hip flexion strength plays an important role in determining the degree of fast gait speed (FGS) post-stroke.20,21 Hemiparetic gait is a common gait abnormality seen post-stroke, characterized by excessive contralesional hip internal rotation, knee extension, and ankle plantar flexion and inversion. This gait can contribute to abnormal compensatory strategies such as hip hiking and/or circumduction during the swing phase.22 These abnormal movements further slow gait and lead to spatiotemporal abnormalities.22
There are many techniques used by physical therapists to address these gait deficits. In particular, strength training is a common rehabilitation tool for individuals post-stroke, due to their observed weakness in the affected extremity.23,24 Historically, there was a hesitancy to treat the hemiparetic side with strength training, as it was thought this type of training could exacerbate symptoms of spasticity in individuals’ post-stroke.25–27 However, resistance training has been demonstrated to increase strength, quality of life and gait speed, and improve functional outcomes without increasing spasticity.28 Additionally, strength training has been shown to decrease the risk of falls as well as decrease length of stay in inpatient settings in individuals post-stroke.29,30 Although strength training for individuals with chronic stroke has been shown to increase strength on the affected side, there is limited evidence to support that strength training alone improves functional walking performance in this population.24
Task-specific training is another technique commonly employed by physical therapists. The technique utilizes high numbers of repetitions to elicit a neuroplastic change.7 However, in order to produce viable change with this method and avoid progression toward abnormal movement patterns, physical therapists need to be able to provide specific cueing which elicits the proper physiologic responses.31,32 Because of the perceived importance of lower extremity muscle strength on gait function, it appears that modifying gait would only be possible if adequate strength was available. Cueing can take various forms including: tactile, haptic, visual, auditory or verbal. Although it has been documented that verbal cueing is common practice during gait rehabilitation, there is little evidence in the literature to support verbal cueing for gait rehabilitation post-stroke independent of resistance training.33
Therefore, the purpose of this study is to determine what effect lower extremity strength has on the amplitude of change in specific functional gait parameters when given specific spatiotemporal verbal cues during gait rehabilitation. Given the role of muscle strength on gait function23,29,30, and the prevalence of lower extremity muscle weakness in individuals post-stroke 2–4; we hypothesize that individuals who produce greater torques, or demonstrate greater strength with manual muscle testing (MMT) will be capable of inducing greater changes in measured gait parameters (i.e. velocity, step length, cadence, symmetry) in response to verbal cues.
Methods
_______________________________________________________________________
Participants
We recruited individuals with chronic (>6 months) stroke from various stroke support groups across North Carolina. Participants were excluded if their stroke occurred in the last 6 months, if the stroke originated from the brainstem or cerebellum, or if the participant demonstrated significant receptive aphasia or other cognitive conditions that hampered the ability to follow directions. Other exclusion criteria included: self-reported uncontrolled cardiorespiratory/metabolic disease (cardiac arrhythmia, uncontrolled hypertension or diabetes, orthostatic hypertension, chronic emphysema), or other neurological or orthopedic disorders that may affect the ability to walk, a history of balance deficits or unexplained falls not related to the stroke, or uncontrolled seizures. Participants were allowed to use their customary footwear, assistive devices, and orthoses during ambulation, but were excluded if they needed anything greater than standby-assist (SBA) from a physical therapist. All participants signed an informed consent form approved by the IRB of the University of North Carolina at Chapel Hill before participating.
Protocol
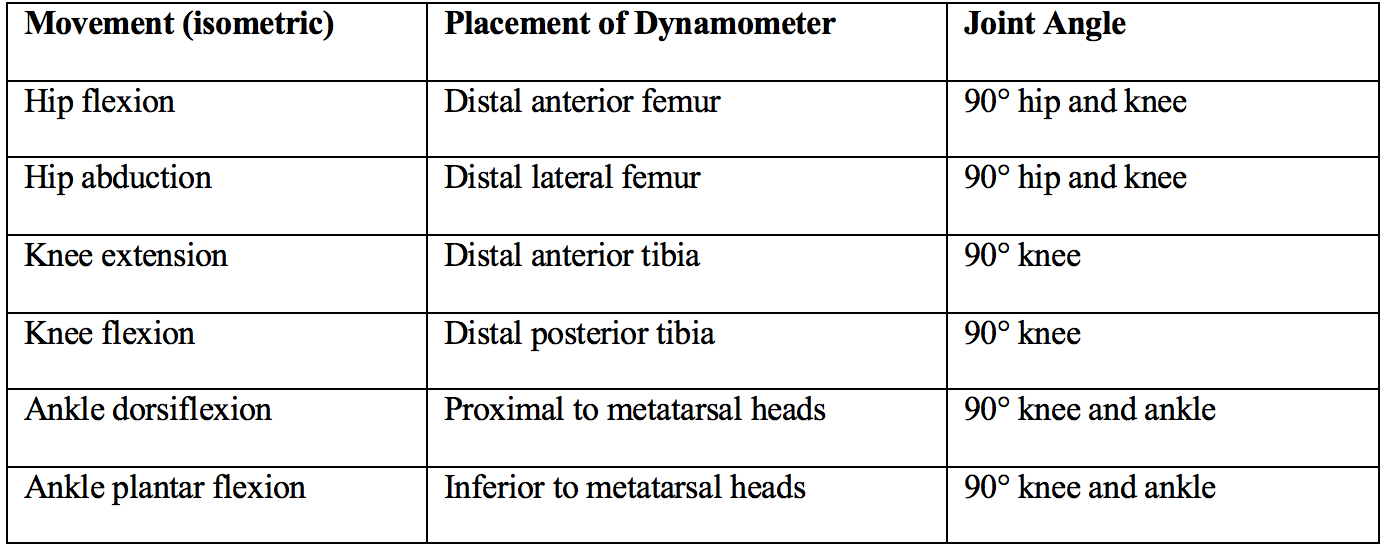
All testing occurred in a single session with the first part consisting of isometric manual muscle testing (MMT) and the second part consisting of gait testing using a 4.27m (14ft) GAITRite mat (CIR systems, Haverford, PA). Approximately 1m at each end of the mat was used for acceleration/deceleration and these data were not recorded. All isometric lower extremity strength was assessed in sitting using a MicroFET 2 hand-held dynamometer (Hoggan Scientific, Salt Lake City, UT). MMT was performed for the following movements: hip flexion (hf), hip abduction (ha), knee flexion (kf), knee extension (ke), ankle dorsiflexion (ad), and ankle plantar flexion (ap). Distance from the active joint (fulcrum) was measured in centimeters using a standard measuring tape, and force was measured in pounds and converted to newtons. This allowed us to calculate joint torque in N·m. The placement of the handheld dynamometer was as follows:
Following the isometric MMT, participants were then instructed to “walk at a comfortable pace” (comfortable gait speed [CGS]) for two passes along the 14ft GAITRite mat. This initial component was used to establish a baseline for the individuals’ gait parameters. The two passes consisted of walking down the mat one way and back the opposite direction. The participant then performed two passes for each of six commands, in random order. The six commands consisted of: (1) “Walk as fast as you can safely”; this was intended to provoke an observable change in velocity of ambulation. (2)“Walk normally, while swinging your arms as much as you can”; this was intended to tap into the coordinated linkage of neural networks between the arm and legs that may be preserved after stroke34 (3)“Walk normally while taking the highest steps that you can”; this was intended to shift weight laterally in order to increase stance time on the paretic limb. (4) “Walk normally, while taking the longest steps that you can”; this was intended to increase step length of both limbs. (5) “Push off of the ground as hard as you can with each step”; this was intended to increase step length of both limbs. (6) “Take the quickest steps that you can”; this was intended to provoke an observable change in the speed of unloading/offloading of both limbs by increasing cadence.
If participants were unable to understand the initial command, it was repeated, but no further explanation or demonstration was given to clarify the instruction. Participants were told before testing that we would only give one command and that it was up to them to interpret that command to the best of their ability.
Data Management and Analysis
Data analysis was performed by GAITRite software which calculated step length, step width, cadence, velocity, stance and swing times of each pass35. Change for each of these parameters was assessed by subtracting the CGS condition from each of the six random commands. We used SPSS (v. 24) to perform statistical analyses of these data. The Pearson correlation coefficient or Pearson’s r was used to measure the linear relationship between strength of each muscle group and the spatiotemporal changes induced with each condition.
Results
_______________________________________________________________________
We successfully recruited and tested 29 participants with unilateral hemiparesis (12 M; 17 F; Age: 63.6 +/- 12.4 years; Height: 1.7m +/- 0.09m; Weight: 83.4 kg +/- 18.5 kg) who were ≥6 months post-stroke with hemiparesis. Of the participants, 14 had right hemiparesis and 15 had left hemiparesis. Twelve of the participants used an ankle-foot-orthosis (AFO) and/or an assistive device such as a single point cane, quad cane or rolling walker.
Among the 29 individuals, significant weakness was observed on the paretic side compared to the non-paretic side for hip flexion, hip abduction, knee flexion, knee extension, ankle plantar flexion, and ankle dorsiflexion moments (all p<0.018; see Figure 1).
Figure 1: Lower Extremity Moments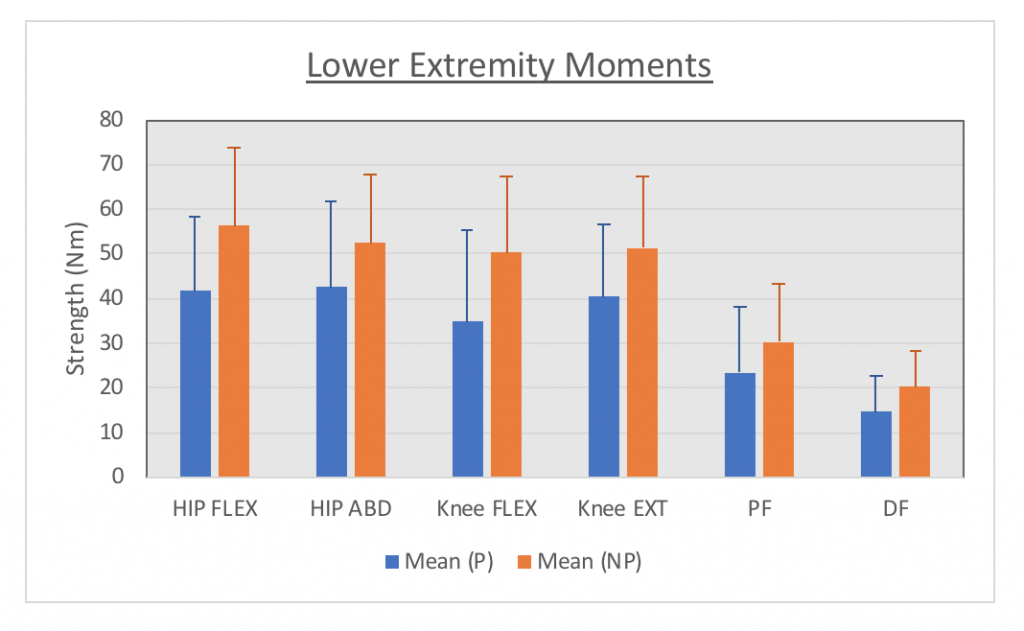 Fig. 1: Shows strength measures taken with the hand-held dynamometer. Blue columns indicate average strength measured on the paretic side; orange columns indicate average strength measured on the nonparetic side. All units are in newton metres indicating torque produced with each given movement.
Fig. 1: Shows strength measures taken with the hand-held dynamometer. Blue columns indicate average strength measured on the paretic side; orange columns indicate average strength measured on the nonparetic side. All units are in newton metres indicating torque produced with each given movement.
In response to verbal cueing, individuals were able to significantly change walking speed. Both verbal cues to “walk as fast as you can safely” and “take as quick of steps as you can” significantly increased walking speed compared to CGS (both p<0.01). With verbal instruction to “walk as fast as you can safely”; we observed that there was a significant relationship between the ability to increase walking speed and the strength of the subject’s paretic knee flexors (p= 0.025; r= 0.415) and paretic dorsiflexors (p= 0.029; r= 0.405). However, with verbal instruction to “take as quick of steps as you can”; we observed no relationship between the ability to increase walking speed and any strength measures (all p>0.136).
Participants also demonstrated an ability to alter cadence. Both verbal cues to “walk as fast as you can safely” and “take as quick of steps as you can” significantly increased walking speed (both p<0.001). With verbal instruction to “take as quick of steps as you can”; we observed that there was a significant relationship between the ability to increase cadence and the subject’s paretic side hip flexion strength (p= 0.021; r= 0.428) and paretic side knee flexion strength (p= 0.019; r= 0.434). With verbal instruction to “walk as fast as you can safely”; we observed no relationship between the ability to increase cadence and any strength measures (all p > 0.115).
Participants also demonstrated the ability to increase step length with the limb initially producing the shorter step length, using verbal cues. In individuals whose shorter step was on the nonparetic side (n=17), knee flexion strength on that side was significantly related to longer step length on the nonparetic side when cued to “walk normally, while taking as long of steps as you can” (p=0.023; r=0.547) and “walk as fast as you can safely” (p=0.011; r=0.600). For individuals whose shorter step was on the paretic side (n=12), knee flexion strength on that side was significantly related to longer step length on that side when cued “walk normally, while taking as long of steps as you can” (p=0.027; r=0.633), “walk as fast as you can safely” (p=0.016; r=0.674), and “walk normally, while swinging your arms as much as you can” (p=0.018; r=0.691). For individuals whose shorter step was on the paretic side (n=12), dorsiflexion strength on that side was significantly related to longer step length on that side when cued to “walk as fast as you can safely” (p=0.050; r=0.576).
Finally, we observed that the paretic sided stance time was modifiable with verbal cueing. Verbal cues to “walk normally while taking as high of steps as you can”, “walk normally, while taking as long of steps as you can” and “push off of the ground as hard as you can with each step” all significantly increased stance time on the paretic limb (all p<0.026). With all three verbal cues, “walk normally while taking as high of steps as you can”, “walk normally, while taking as long of steps as you can” and “push off of the ground as hard as you can with each step,” we observed no relationship between the ability to increase stance time on the paretic limb and any strength measures (all p > 0.126).
Discussion
_______________________________________________________________________
Our hypothesis that individuals who demonstrate greater strength will produce greater changes in gait parameters with verbal cueing, was partially supported by these data. Participants were able to increase walking speed, cadence, and step lengths with significant correlation to limb flexor strength measures. Despite the relationship between paretic knee flexor strength and the ability to change gait speed, cadence, and step length, there were other gait parameters that were altered in response to verbal cues that had no relationship to lower extremity strength. For example, using the cue to “take as quick of steps as you can” increased walking speed independent of the individual’s strength measures. Using the cue to “walk as fast as you can safely” increased cadence independent of strength measures. And finally, using all three verbal cues, “walk normally while taking as high of steps as you can”, “walk normally, while taking as long of steps as you can” and “push off of the ground as hard as you can with each step,” increased paretic stance time independent of strength measures. This may indicate that limb flexion strength may be important for altering gait parameters during some verbal cues, whereas walking speed, cadence and paretic side stance time can also be improved independent of lower extremity strength.
Clearly, some strength measures played a significant role in improving walking speed, cadence and step length in response to verbal cues. For instance, participants with greater knee flexor and ankle dorsiflexor strength had an increased ability to improve walking speed when asked to “walk as fast as you can safely”. Participants with greater hip flexor and knee flexor strength had an increased ability to improve cadence when asked to “take as quick of steps as you can”. Participants with greater knee flexor strength had an increased ability to improve step length on the nonparetic side when asked to “walk normally, while taking as long of steps as you can” and “walk as fast as you can safely”. Participants with greater knee flexor strength had an increased ability to improve step length on the paretic side when asked to “walk normally, while taking as long of steps as you can” and “walk as fast as you can safely”. Finally, participants with greater ankle dorsiflexor strength had an increased ability to improve step length on the paretic side when asked to “walk as fast as you can safely”.
From a clinical perspective, these results indicate some promising outcomes for participants undergoing gait rehabilitation post-stroke. First, this reinforces previous literature of the importance of strengthening residual knee flexion36, hip flexion20,33 and ankle dorsiflexion33 post-stroke in order to preserve and improve walking speed, cadence, and step length. The improvement of hip flexion strength and endurance has been shown to compensate for decreased propulsive forces lower in the chain, at the knee and ankle, that contribute to gait abnormality, fatigue and decreased walking speed.37 The improvement of knee flexion and ankle dorsiflexion strength has been shown to make a key contribution to increased foot height and toe clearance during the swing phase of the gait cycle contributing to a decreased chance of falls.38 In addition, lower limb flexors are typically the most affected post-stroke as evidenced in Figure 1, possibly because flexors in the lower extremity tend to be intrinsically weaker than extensors.39 By preserving and strengthening residual hip flexion, knee flexion and ankle dorsiflexion, an individual may be able to elicit greater changes in walking speed, cadence and step length with verbal cues.
Secondly, for those with less residual strength in the hemiparetic limb, this study shows that strength deficits can be circumvented through the proper verbal cues. Although multiple verbal cues can be used to elicit a positive rehabilitative gait response in participants with post-stroke hemiparesis, certain cues can elicit this response independent of the degree of lower extremity strength. For instance, using both the cues “walk as fast as you can safely” and “take as quick of steps as you can” both elicited increased walking speed. However, only the cue to “take as quick of steps as you can” elicited increased walking speed independent of an individual’s strength.
We know from previous literature that cueing during gait retraining is superior to gait training alone in improving walking speed, cadence, step length and symmetry,40 indicating that cueing is an important and necessary aspect of gait retraining post-stroke. Our work extends this evidence to suggest that improvements in gait parameters from verbal cueing may be possible independent of the degree of strength that the participant possesses.
One limitation to this study was the varying degree of comprehension of commands that existed between participants. Because of our intention to isolate a specific verbal cue, we could not modify or individualize each command for better subject comprehension. Therefore, there was some variation in interpretation of each command. This was especially evident with the commands to “push off the ground as much as you can with each step” and “walk normally, while swinging your arms as much as you can”. Another limitation was the variation in the time since stroke that existed between subjects. The chronicity of stroke duration ranged from 6 months to 25 years which may have affected the outcome of certain commands based on subjects’ familiarity with therapy and previous gait-training. Not only did participants vary in the chronicity of their stroke, but they also varied with what assistive devices and orthoses they used. Twelve of the twenty-nine subjects used some form of assistive device, AFO or combination. Nine subjects used a single-point cane, 5 subjects used AFOs, 2 subjects a RW or Rollator, and 1 subject a quad cane. Another limitation to this study was that the degree of change in each gait parameter was measured as an immediate effect of each verbal command, we did not take into consideration how these verbal commands may affect gait rehabilitation long-term.
Future studies may address some of these limitations by customizing verbal commands to address differences in comprehension as well as include visual demonstration in order to mimic more realistic clinical scenarios. Future studies may also include only participants within a particular range of time post-stroke and/or those requiring a specified amount of assistance. Future longitudinal studies may benefit from measuring the long-term effects verbal cues have on gait parameters post-stroke in order to provide more evidence to what verbal cues create more long-lasting change. Future longitudinal studies may benefit from examining the effect of strengthening of lower limb flexors because, although our study shows a positive relationship between hip flexion, knee flexion, and ankle dorsiflexion strength, we did not directly measure the effects of improving strength or control with these muscles. Furthermore, this study only looked at six distinct verbal cues; future studies will benefit by examining if other types of verbal cues have similar or differing effects. Finally, greater detail into the nature of stroke, such as lesion location or artery involvement, may pinpoint the underlying mechanisms responsible for these results.
- Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017;135(10):e146-e603. doi:10.1161/CIR.0000000000000485.
- Langhorne P, Stott DJ, Robertson L, et al. Medical complications after stroke: a multicenter study. Stroke 2000;31(6):1223-1229. doi:10.1161/01.STR.31.6.1223.
- Ramnemark A, Nilsson M, Borssén B, Gustafson Y. Stroke, a major and increasing risk factor for femoral neck fracture. Stroke 2000;31(7):1572-1577.
- Weerdesteyn V, de Niet M, van Duijnhoven HJR, Geurts ACH. Falls in individuals with stroke. J Rehabil Res Dev 2008;45(8):1195-1213.
- Bohannon RW, Andrews AW, Smith MB. Rehabilitation goals of patients with hemiplegia. International Journal of Rehabilitation Research 1988;11(2):181-184. doi:10.1097/00004356-198806000-00012.
- Lang CE, MacDonald JR, Gnip C. Counting Repetitions: An Observational Study of Outpatient Therapy for People with Hemiparesis Post-Stroke. J Neurol Phys Ther 2007;31(1):3-10. doi:10.1097/01.NPT.0000260568.31746.34.
- Lang CE, Macdonald JR, Reisman DS, et al. Observation of amounts of movement practice provided during stroke rehabilitation. Arch. Phys. Med. Rehabil. 2009;90(10):1692-1698. doi:10.1016/j.apmr.2009.04.005.
- Jette DU, Latham NK, Smout RJ, Gassaway J, Slavin MD, Horn SD. Physical therapy interventions for patients with stroke in inpatient rehabilitation facilities. Phys. Ther. 2005;85(3):238-248. doi:10.1093/ptj/85.3.238.
- Holleran CL, Straube DD, Kinnaird CR, Leddy AL, Hornby TG. Feasibility and potential efficacy of high-intensity stepping training in variable contexts in subacute and chronic stroke. Neurorehabil. Neural Repair 2014;28(7):643-651. doi:10.1177/1545968314521001.
- Raja B, Neptune RR, Kautz SA. Quantifiable patterns of limb loading and unloading during hemiparetic gait: Relation to kinetic and kinematic parameters. J Rehabil Res Dev 2012;49(9):1293-1304.
- Sackley CM. Falls, sway, and symmetry of weight-bearing after stroke. Int Disabil Stud 1991;13(1):1-4.
- Dean JC, Kautz SA. Foot placement control and gait instability among people with stroke. J Rehabil Res Dev 2015;52(5):577-590. doi:10.1682/JRRD.2014.09.0207.
- Lewek MD, Bradley CE, Wutzke CJ, Zinder SM. The relationship between spatiotemporal gait asymmetry and balance in individuals with chronic stroke. J Appl Biomech 2014;30(1):31-36. doi:10.1123/jab.2012-0208.
- Sullivan KJ, Brown DA, Klassen T, et al. Effects of task-specific locomotor and strength training in adults who were ambulatory after stroke: results of the STEPS randomized clinical trial. Phys. Ther. 2007;87(12):1580-1602. doi:10.2522/ptj.20060310.
- Schindler-Ivens S, Desimone D, Grubich S, Kelley C, Sanghvi N, Brown DA. Lower extremity passive range of motion in community-ambulating stroke survivors. J Neurol Phys Ther 2008;32(1):21-31. doi:10.1097/NPT.0b013e31816594ea.
- Bonnyaud C, Pradon D, Vaugier I, Vuillerme N, Bensmail D, Roche N. Timed Up and Go test: Comparison of kinematics between patients with chronic stroke and healthy subjects. Gait Posture 2016;49:258-263. doi:10.1016/j.gaitpost.2016.06.023.
- Chen G, Patten C, Kothari DH, Zajac FE. Gait differences between individuals with post-stroke hemiparesis and non-disabled controls at matched speeds. Gait Posture 2005;22(1):51-56. doi:10.1016/j.gaitpost.2004.06.009.
- Phan PL, Blennerhassett JM, Lythgo N, Dite W, Morris ME. Over-ground walking on level and sloped surfaces in people with stroke compared to healthy matched adults. Disabil. Rehabil. 2013;35(15):1302-1307. doi:10.3109/09638288.2012.729646.
- Kim CM, Eng JJ, Whittaker MW. Level walking and ambulatory capacity in persons with incomplete spinal cord injury: relationship with muscle strength. Spinal Cord 2004;42(3):156-162. doi:10.1038/sj.sc.3101569.
- Hsu A-L, Tang P-F, Jan M-H. Analysis of impairments influencing gait velocity and asymmetry of hemiplegic patients after mild to moderate stroke. Arch. Phys. Med. Rehabil. 2003;84(8):1185-1193.
- Lin P-Y, Yang Y-R, Cheng S-J, Wang R-Y. The relation between ankle impairments and gait velocity and symmetry in people with stroke. Arch. Phys. Med. Rehabil. 2006;87(4):562-568. doi:10.1016/j.apmr.2005.12.042.
- Neckel ND, Blonien N, Nichols D, Hidler J. Abnormal joint torque patterns exhibited by chronic stroke subjects while walking with a prescribed physiological gait pattern. J Neuroeng Rehabil 2008;5:19. doi:10.1186/1743-0003-5-19.
- Wist S, Clivaz J, Sattelmayer M. Muscle strengthening for hemiparesis after stroke: A meta-analysis. Ann Phys Rehabil Med 2016;59(2):114-124. doi:10.1016/j.rehab.2016.02.001.
- Eng JJ. Strength Training in Individuals with Stroke. Physiother. Can. 2004;56(4):189-201.
- Sharp SA, Brouwer BJ. Isokinetic strength training of the hemiparetic knee: effects on function and spasticity. Arch. Phys. Med. Rehabil. 1997;78(11):1231-1236.
- Ada L, Vattanasilp W, O’Dwyer NJ, Crosbie J. Does spasticity contribute to walking dysfunction after stroke? J. Neurol. Neurosurg. Psychiatry 1998;64(5):628-635.
- Bobath B. Adult Hemiplegia Evaluation and Treatment. 3rd ed. Butterworth-Heinemann; 1990.
- Pak S, Patten C. Strengthening to promote functional recovery poststroke: an evidence-based review. Top Stroke Rehabil 2008;15(3):177-199. doi:10.1310/tsr1503-177.
- Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol 1989;44(4):M112-7.
- Andrews AW, Bohannon RW. Discharge function and length of stay for patients with stroke are predicted by lower extremity muscle force on admission to rehabilitation. Neurorehabil. Neural Repair 2001;15(2):93-97. doi:10.1177/154596830101500202.
- Lewek MD, Braun CH, Wutzke C, Giuliani C. The role of movement errors in modifying spatiotemporal gait asymmetry post stroke: a randomized controlled trial. Clin. Rehabil. 2018;32(2):161-172. doi:10.1177/0269215517723056.
- Johnson L, Burridge JH, Demain SH. Internal and external focus of attention during gait re-education: an observational study of physical therapist practice in stroke rehabilitation. Phys. Ther. 2013;93(7):957-966. doi:10.2522/ptj.20120300.
- States RA, Pappas E, Salem Y. Overground physical therapy gait training for chronic stroke patients with mobility deficits. Cochrane Database Syst. Rev. 2009;(3):CD006075. doi:10.1002/14651858.CD006075.pub2.
- Zehr EP, Hundza SR, Vasudevan EV. The quadrupedal nature of human bipedal locomotion. Exerc Sport Sci Rev 2009;37(2):102-108. doi:10.1097/JES.0b013e31819c2ed6.
- Lewek MD, Randall EP. Reliability of spatiotemporal asymmetry during overground walking for individuals following chronic stroke. J Neurol Phys Ther 2011;35(3):116-121. doi:10.1097/NPT.0b013e318227fe70.
- Eng JJ, Tang P-F. Gait training strategies to optimize walking ability in people with stroke: a synthesis of the evidence. Expert Rev Neurother 2007;7(10):1417-1436. doi:10.1586/14737175.7.10.1417.
- Rybar MM, Walker ER, Kuhnen HR, et al. The stroke-related effects of hip flexion fatigue on over ground walking. Gait Posture 2014;39(4):1103-1108. doi:10.1016/j.gaitpost.2014.01.012.
- Roche N, Bonnyaud C, Geiger M, Bussel B, Bensmail D. Relationship between hip flexion and ankle dorsiflexion during swing phase in chronic stroke patients. Clin. Biomech. (Bristol, Avon) 2015;30(3):219-225. doi:10.1016/j.clinbiomech.2015.02.001.
- Thijs RD, Notermans NC, Wokke JH, van der Graaf Y, van Gijn J. Distribution of muscle weakness of central and peripheral origin. J. Neurol. Neurosurg. Psychiatry 1998;65(5):794-796.
- Nascimento LR, de Oliveira CQ, Ada L, Michaelsen SM, Teixeira-Salmela LF. Walking training with cueing of cadence improves walking speed and stride length after stroke more than walking training alone: a systematic review. J Physiother 2015;61(1):10-15. doi:10.1016/j.jphys.2014.11.015.
PDF Version: **CAPSTONE III***
Image source: https://nsistemcell.com/news-about-stem-cell-therapy-for-stroke/


2 Responses to “The Effects of Lower Extremity Strength on Verbal Cueing Response in Gait Rehabilitation Post-Stroke”
Michael Lewek
Ben
Nice job pulling this together. You did an especially good job or summarizing lots of information in a ‘simpler’, but meaningful way. In my response to Hailey’s post I indicated how you can tell the level of asymmetry present in your tested subjects (although I’m not sure that those results were present in your output – only Hailey’s).
Nice job.
Mike
Vicki Mercer
Hi Ben!
Good work on this project! I really like the table you have at the end summarizing the “points of clinical importance”. I have a couple of questions for both you and Hailey – How much spatiotemporal gait asymmetry did your participants demonstrate? How did they compare in this regard with participants with stroke from other studies reported in the literature (i.e., were they typical for people post stroke who are able to ambulate independently?)?
Vicki