Scapular Taping for Subacromial Impingement in Overhead Athletes
By Matthew Medlin

Overview
When I pitched for the Atlanta Braves (see above) I definitely struggled with subacomial impingement. In fact, subacromial impingement is the most common form of shoulder pathology in overhead athletes and nonathletic populations (Kumar 2012, Jobe 2000). Reported incidence rates can climb as high as 42% in some athletic populations (Lewis 2005).
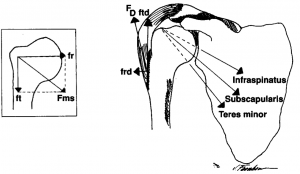
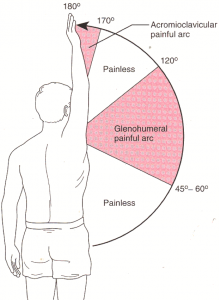
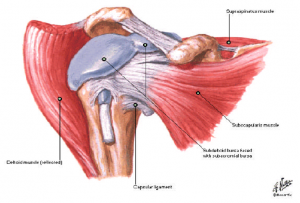
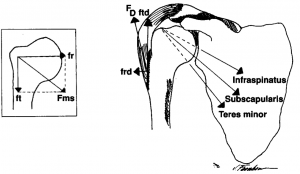
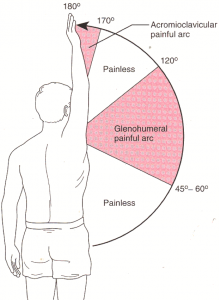
It is characterized by compression of structures that reside within the subacromial space, including: supraspinatus tendon, biceps tendon long head and subacromial bursa. The supraspinatus tendon is particular at riks as a result of its proximity and likelihood to contact the acromion when the humerus is abducted to 90 degrees and internally rotated to 45 degrees.
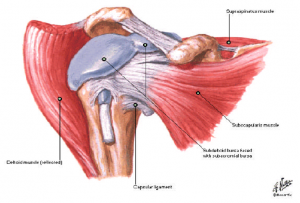
Many studies suggest that subacromial impingement is strongly related to muscle imbalances, particularly weakness in the lower and middle trapezius and serratus anterior with tightness presenting in the upper trapezius fibers and anterior structures (i.e. pectorals). Consequently, scapular elevation and decreased posterior tilt, external rotation and upward rotation results. This is particularly problematic for overhead athletes where repetitive overhead activity results in increasing wear and tear on subacromial structures, leading to degenerative changes and risk for injury.
Below is an excellent video demonstrating Type I scapular dyskinesia in an elite swimmer, which is typically considered an early sign of shoulder pathology. It is characterized by tightness of the anterior structures and weakness of the lower trapezius fibers and serratus anterior. As a result, functional narrowing of the subacromial space occurs with overhead motion, creating pain with abduction.
[youtube]http://www.youtube.com/watch?v=HRalJc5T_5g&list=PL2D62BC8334090A5F[/youtube]
Since I am particularly interested in shoulder pathology (and let’s be honest, many of your are not), I decided to create a project that helps to educate ALL OF YOU! My hope is that it is basic enough to facilitate an improved understanding among even the most novice PTs, as well as up-to-date and strong enough to help complement experienced therapists’ body of knowledge.
Why Scapular Taping?
Many interventions utilized to address SIS do not result in facilitating the permanent change and reduced pain that many athletes desire. Therefore, physical therapy is often a very efficacious option to help manage symptomatic individuals. Obviously, exercise is probably the most often considered tool in these populations. Yet, even exercise is not always tolerated, nor effective for every patient. Moreover, even with very conscious effort some movement activation patterns simply cannot be corrected (Michener 2004, Reinold 2004).
Scapular taping hypothesized mechanisms for improvement include: enhanced joint stability, improved strength, improved proprioception, enhanced muscle activation patterns, pain reduction, and scapular re-positioning (Hsu 2009, Williams 2012).
Therefore, my question is: Does inclusion of scapular taping enhance effectiveness of rehabilitation for subacromial impingement in overhead athletes?
Literature Review
To help develop an answer to my question, a strong literature review was warranted. To assess the effectiveness of scapular taping protocols, I researched studies that considered outcomes based on taping methods ALONE vs. rehabilitation regimens that were comprehensive and included use of taping as a complementary therapy. The results can be reviewed in my Evidence Table.
Through my literature appraisal, I consider scapular taping and its effects on a multitude of proposed mechanisms. Moreover, I provide great detail on the differences among techniques and variable application protocols. You can access that information in my Capstone PowerPoint. This final material was developed and altered from feedback provided that is compiled here. Combined with that, in order to maximize the effectiveness of my powerpoint, I used many Chiara Ojeda suggestions, including utilization of pictures, simplification of slides, improved color integration and use of color contrast, and elimination of excessive wording. You can compare the final product changes to my initial Capstone PDF and judge for yourself.
Your Lucky Day
On top of all that, I also incorporated basic assessment and evaluation tools, including historical signs and symptoms to look for, special tests interpretation, and outcome measures that are considered pscyhometrically appropriate for athletic populations. I would love any feedback that anybody would like to provide on ways in which I can improve my powerpoint. And DO NOT FORGET, I MADE THIS FOR YOU GUYS TO USE, so do so, and let me know how it goes! Use this feedback form to help direct me in further developing this project! I have already received some feedback, which I will compile and add as we get closer to the final date. Thanks guys! (Go Braves!)
Feedback Form
Special Thanks to all those who have provided invaluable feedback throughout my evidence search, material production and evaluation. Thanks to Mike McMorris, Mike Gross, Pamela Elske-Leonetti, Kyle Hoppes, Nick Camilleri, Mijo Cotic and Brandon Lindquist. I appreciate any and all time and consideration given to make my project the best possible.
References
2.Fongermie, AE. Management of shoulder impingement syndrome and rotator cuff tears. Am Fam Physician. 1998 Feb;57(4):667-74, 680-2.
3.Hawkins, RJ and Kennedy, JC. Impingement syndrome in athletes. Am J Sports Med. June 1980 vol. 8 no. 3 151-158.
4.Selkowitz, D; Chaney, C; Stuckey, SJ; Vlad, G. The Effects of Scapular Taping on the Surface Electromyographic Signal Amplitude of Shoulder Girdle Muscles During Upper Extremity Elevation in Individuals With Suspected Shoulder Impingement Syndrome. JOSPT. 2007 Nov; 37 (11): 694-702.
5.Kumar, NSS; Nehru, A; Rajalakshmi, D. Effect of taping as component of conservative treatment for subacromial impingement syndrome. Health: Scientific Research. 2012;4(4): 237-241.
6.Page, P. Shoulder Muscle Imbalance and Subacromial Impingement Syndrome In Overhead Athletes. Int J Sports Phys Ther. 2011 Mar;6(1): 51-58.
7.Jobe, CM; Coen, MJ; Screnar, P. Evaluation of impingement syndromes in the overhead-throwing athlete. J Athl Train, 2000;35: 293–299.
8.Hsu Y, Chen W, Wang W, Shih Y.
The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. Journal of Electromyography and Kinesiology. 2009;19(6):1092-1099.
9.Williams S, Whatman C, Hume P, Sheerin K. Kinesio Taping in Treatment and Prevention of Sports Injuries. Sports Medicine. February 2012;42(2):153-164.
10.McConnell, J; Donnelly, C; Hamner, S; Dunne, J; Besler, T. Effect of shoulder taping on maximum shoulder external and internal rotation range in uninjured and previously injured overhead athletes during a seated throw. J Ortho Research. 2011; 29(9): 1406-1411.
11.Thelen, Mark D. The clinical efficacy of kinesio tape for shoulder pain: a randomized, double-blinded, clinical trial. JOSPT. 2008; 38 (7), 389.
12.Host, H. Scapular taping in the treatment of anterior shoulder impingement. Physical Therapy. 1995;75(9): 27.
13.Cools, AM; Witvrouw, EE; Danneels, LA; Cambier, DC. Does taping influence electromyographic muscle activity in healthy shoulders? Man Ther. 2002 Aug;7(3):154-62
14.Tucker W.S., Armstrong C.W., Gribble P.A., Timmons M.K., Yeasting R.A. Scapular Muscle Activity in Overhead Athletes With Symptoms of Secondary Shoulder Impingement During Closed Chain Exercises. Archives of Physical Medicine and Rehabilitaiton. 2010; 91 (4), 550-556.
15.Smith, MJ; Sparkes, V. The immediate effect of scapular taping on surface electromyographic activity of the scapular rotators in swimmers with subacomial impingement syndrome. PT in Sport. 2006; 7(14): 171.
16.Lewis, JS; Wright, C; Green, A. Subacromial Impingement Shoulder: The Effect of Changing Posture on Shoulder Range of Movement. JOSPT. 2005; 35(2): 72-87.
17.Scmitt, L; Synder-Mackler, L. Role of Scapular Stabilizers in Etiology and Treatment of Impingement Syndrome. JOSPT. 1999; 29(1): 31-38.
18.Kaya, E; Zinnuroglu, M; Tugcu, I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clin Rheumatol. 2011; 30: 201-207.
19.Cools AM, Dewitte V, Lanszweert F, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007;35(10): 1744-1751.
20.Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg. 2009; 18(1): 138-160.
21.De Mey, K; Danneels, L; Cagnie, B; Cools, AM. Scapular Muscle Rehabilitation Exercises in Overhead Athletes With Impingement Symptoms: Effect of a 6-Week Training Program on Muscle Recruitment and Functional Outcome. Am J Sports Med. 2012: 40(8): 1906-1915.
22.Koester, MC; Dunn, WR; Kuhn, JE; Spindler, KP. The Efficacy of Subacromial Corticosteroid Injection in the Treatment of Rotator Cuff Disease: A Systematic Review. J Am Acad Orthop Surg. 2007; 15: 3-111.
24.Buchbinder, R; Green, S; Youd, JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev. 2003; (1): CD004016.
25.Michener, LA; Walsworth, MK; Burnet, EN. Effectiveness of Rehabilitation for Patients with Subacromial Impingement Syndrome. J Hand Ther. 2004; 17: 152-164.
26.Hacke, Jon. The Shoulder Complex. PHYT 732: Musculoskeletal I. University of North Carolina at Chapel Hill. Accessed February 25, 2013.
27.Hacke, Jon. Impingement Syndrome. PHYT 732: Musculoskeletal I. University of North Carolina at Chapel Hill. Accessed February 25, 2013.
28.Hacke, Jon. Shoulder Lab Handout. PHYT 732: Musculoskeletal I. University of North Carolina at Chapel Hill. Accessed February 13, 2013.
29.Reinold, MM; Wilk, KE; Fleisig, GS; et al. Electromyographic Analysis of The Rotator Cuff and Deltoid Musculature During Common Shoulder External Rotation Exercises. JOSPT. 2004 Jul; 34(7): 385-394.
31.McConnell Taping Technique. Orthopedic Physical Therapy Products Newsletter. May 2006.
32.Alberta, FG; ElAttrache, NS; Bissell, S; Mohr, K; Browdy, J; Yocum, L; Jobe, F. The Development and Validation of a Functional Assessment Tool for the Upper Extremity in the Overhead Athlete. Am J Sports Med. 2010 Mar; 38(5): 903-911.
33.Krishnan, SG; Hawkins, RJ; Warren, RF. The Shoulder and the Overhead Athlete. 2004 by Lippincott Wiliams & Wilkins. Philadelphia, PA.
34.Bas de Witte, P; Henseler, JF; Nagels, J; Vlieland, TPMV; Nelissen, RGHH. The Western Ontario Rotator Cuff Index in Rotatr Cuff Disease Patients: A Comprehensive Reliability and Responsiveness Validation Study. Am J Sports Med. 2012 May; 40(7): 1611-1619.
35.Breckenridge, JD; McAuley, JH. Shoulder Pain and Disability Index (SPADI). J Physiother. 2011; 57(3): 197.


4 Responses to “Scapular Taping for Subacromial Impingement in Overhead Athletes”
Mike Gross
Matt- nice work on your project. What was missing for me in looking at your presentation was the specific rationale for each of the taping configurations and then the research results that would speak specifically to each intended purpose. For example, is the strip of tape designed to improve scapulotharacic position/mechanics and are there radiographic/dynaic flouroscopy data to suuport the contention? Is the strip of tape designed to increase subacromial space and are there data to support this. is the strip of tape designed to improve muscle activation, through what mechanicsm, and are there EMG data and other data to support this? Otherwise, very nice work? You might think of coming up with an assessment tool that would identify the presence of issues that might be addressed with taping. Mike Gross
mmedlin
Paige and Cassie, thanks for you questions and kind words!
Paige, through my research I was able to find very little evidence on actual use during sporting activities. Most of my evidence exists on the efficacy and effectiveness of such in rehabilitation settings post-injury. However, McConnell demonstrates use of taping during a overhead throwing task and found that it did indeed impact ROM at the GHJ but did not show changes in ball throwing velocity. However, this was in produced in a very limited task compared to the rigorous nature of elite level performance. Moreover, my search was focused on the effects for use of taping at the scapula, whereas many of the Kinesio taping techniques that are prevalent among today’s athletes APPEAR from my point of view to be less often utilized in that respect. Furthermore, as you mention, beneficial effects were definitely seen to decrease as time increased. Many of my studies, (Williams, Kumar, etc.) demonstrate that changes are very short-lived and require significant reassessment/retaping protocols. Also, for the most part, to remove bias, many of my studies removed adjunctive exercise therapy or significant participation in sports in order to focus solely on changes achieved by scapular taping. Thus, identification for effectiveness in athletic participation was difficult to determine from my results.
Cassie, from my research, IF (and a big if) scapular taping is to work, it would only likely be useful in addition to strengthening exercises and other rehabilitation tools such as modalities and stretching. From what I gather there is no specific protocol for use of taping. Therefore, you will have to rely on your astute clinical judgment for application based on individual patient preferences. Although sending a person home with tape still on is an option, there is definitely concern that effects of taping are not likely to be significant following the very short term after application. Yet, in some instances it could be beneficial, in my opinion. For example, although the taping may provide no actual tangible improvement, perhaps it provides a gentle reminder to sit with improved posture? For me, depending on the patient’s presentation, use of taping will vary. Individuals with significant kinematic alterations would be much more likely to benefit from increased wear time, especially during exercises if they are unable to correct mechanics consciously. If the individual is able to perform tasks soundly, use of taping may be more beneficial after exercises have been performed. Overall, again, I think your judgment and evaluation will play a huge role if you decide to use this tool.
clshort
Hi Matt!!
First of all, I laughed for about 15 minutes after reading the first sentence of your page (I also shared it with Tim). Anyways- I just wanted to congratulate you on a job well done with your project. I have to say about 80% of the patients I’ve seen with shoulder problems, have had subacromial impingement (athlete or not). I have never had the opportunity to use taping as an intervention, and I really enjoyed learning more about it through your research and materials.
I have heard of the McConnell technique that you mentioned, but for PFPS- So I didn’t know that it was used for multiple joints! I was thinking about how I would use this when a patient comes in for follow-up treatments- tape them, perform exercises (ROM/strength), have them leave with it still on and remove the tape before going to bed? Is this accurate? I know skin irritation can occur if left on more than 18 hours, but would you suggest this method of sending patients home with taping (instructing them to take it off before bed) is ok? If they are coming in 2-3 days per week, I suppose every other day of taping would really benefit in combination with their HEP and therapy.
Great job!
Cassie
ekensrue
Hi Matt!
Thanks for the great information about taping! I feel as though this has become such a “hot topic” is sports medicine in the last ten years with taping seen on professional athletes during competitions and in the Olympics. I appreciate the depth that your presentation materials gave, including the background behind what an impingement diagnosis presents like and then why taping is thought to work for this type of pathological process. I will definitely use your materials as a resource when I work with overhead athletes with impingement.
I was wondering if you found in your research if there was a certain protocol that researchers used for the taping (i.e. can you initiate taping the first day of treatment and then how long should you continue using taping)? I also wondered if you found any effects on sport performance with taping? I see these athletes wearing the tape during competition, but I also wonder what exactly it is doing for them seeing as research has previously shown that ankle taping loses its beneficial effects after about 30 minutes. I understand that the tape material itself is different, but can it sustain the elements of competition?
Thanks again for this information!
Paige