Multidirectional Instability and Ehlers-Danlos Syndrome:
Evaluation and Treatment of the Shoulder
Jessica Rolle, SPT
Spring 2014
1
Overview of MDI and EDS
My initial interest in this topic stemmed from my younger sister’s diagnosis of Ehlers-Danlos syndrome (EDS) about 10 years ago. She has had numerous shoulder subluxations and dislocations throughout her life and has learned to manage her condition with the help of physical therapy.
Ehlers-Danlos syndrome is a relatively rare, inherited connective tissue disorder. It is characterized by skin extensibility, tissue fragility, and joint hypermobility due to ligamentous laxity. These patients have joint hypermobility throughout their body, but the shoulder is one joint that is especially vulnerable to injury. As physical therapists, we are likely to see these patients after a shoulder subluxation or dislocation, and we must take their underlying EDS diagnosis into account when developing a treatment plan.
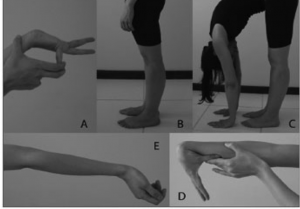
Global hypermobility can be quantified using the Beighton Score, which is depicted here:
A = passively dorsiflex the fifth metacarpophalangeal joint to >90 degrees (0-2 points)
B = hyperextend the knee to >10 degrees (0-2 points)
C = place hands flat on the floor without bending the knees (0-1 point)
D = oppose the thumb to the volar aspect of the ipsilateral forearm (0-2 points)
E = hyperextend the elbow to >10 degrees (0-2 points)
**A score of 5/9 or greater is indicative of generalized joint hypermobility.
Multidirectional instability (MDI) is another cause of atraumatic shoulder instability in which patients have increased glenohumeral motion in more than one direction. These patients are also at an increased risk of shoulder injury.
The most critical component of treatment for these patients with either EDS or MDI is neuromuscular re-education. Since the static stabilizers of the shoulder are unable to adequately support the glenohumeral joint, the surrounding muscles must provide extra stability. Physical therapists should implement exercises targeting proprioception and control throughout the patient’s full range of motion. Exercises should incorporate closed chain activities to facilitate co-contractions as well as general strengthening of the shoulder complex with low resistance and high repetitions. Finally, it is important to restore scapular and glenohumeral motion by identifying and treating any soft tissue restrictions.
Project
I gave a presentation to 30 first year students in their Musculoskeletal I class, as well as 6 second and third year students and 2 faculty members. I encouraged the first years to fill out an evaluation form at the conclusion of my lecture, and here is the combined feedback.
Additionally, I compiled my research into an evidence table and summarized my information in a review paper.
Acknowledgments
A big thank you goes to my committee members, Mike McMorris and Rob Woodside, as well as my advisor, Mike Gross. I would also like to thank my sister, Meaghan Rolle, for her willingness to be a part of my project and her desire to educate others about her condition. Finally, thank you to the first year students who were a great audience!
Photos:
1. http://www.sportsinjuryclinic.net/sport-injuries/shoulder-pain/dislocated-shoulder
2. Pasinato F, Souza JA, Correa ECR, da Silva AMT. Temporomandibular disorder and generalized joint hypermobility: application of diagnostic criteria. Braz J Otorhinolaryngol. 2011;77(4):418-425.
3. http://www.perfectlyfitonline.com/2010/11/basic-exercise-for-serratus-anterior/
4. http://www.youtube.com/watch?v=ywsxrw-VZ7g.




3 Responses to “MDI and EDS: Evaluation and Treatment”
Jess Rolle
Hi Meredith!
Thanks for your comments and great questions! An important thing to consider when performing passive range of motion is the patient’s tolerance to the movement. Many times these patients will have pain prior to subluxation. By looking at their facial expressions and reactions to the PROM, you can determine an appropriate stopping point. Some patients may not have as much discomfort with PROM or their pain tolerance is much higher. In these cases, I would suggest stretching them through the “normal” ROM, but not into their hypermobile range. Once the patient is able to get full normal ROM, it is unnecessary to stretch past this as you then begin to place the shoulder in a more vulnerable position for subluxation. To answer your second question about subluxation during therapy, it depends on whether the patient has had a subluxation before and the patient’s current response. For example, if my sister were to sublux her shoulder today, she would just reduce it on her own and continue with her daily activities. She may be sore for the next few days and have trouble lifting heavy objects, but this injury would not cause significant problems for her. In the clinic, I would probably stop exercises for the day, make sure the shoulder had reduced appropriately, and apply ice, as you suggested. This injury may cause a slight setback in your overall plan of care, but can be adequately treated with PT. And, of course, it is important to document how the subluxation occurred and how you (and the patient) responded to the situation. Interestingly, my dad and grandmother (dad’s mother) both have EDS as well. Unfortunately my dad’s symptoms are more severe than my grandmother’s, and my sister’s symptoms are more severe than my dad’s.
Thanks again for the post!
Jess
Meredith Haigh
Hey Jess!
I’ve been really excited to read about your capstone after hearing about your sister’s diagnosis earlier this year. You did a really great job! Your paper and presentation were both a really great review of the shoulder anatomy, evaluation techniques, and treatment ideas. Thank you! I remember during my very first clinical, we had a few patients with shoulder instability and I remember my CI teaching me how to do some of the treatment techniques that you mentioned like isometric contractions and range of motion through the scapular plane. One question that I have is when performing passive range of motion, how do you know how far you can go without causing a subluxation? Also, what should you do if you DO cause a subluxation or if the shoulder subluxes during a therapy session? Should you stop activities for the day and switch to modalities?
Also, about your sister, you mentioned that EDS is hereditary. Do either of your parents have EDS? Or anyone else in your family?
You got some great feedback and I totally agree, excellent job! I learned a lot! Thank you!
Meredith Haigh
Mike McMorris
Jess,
Great job on your capstone! Really appreciate you coming in to speak to the 1st year class about shoulder instability in general as well as in patients with EDS. Congrats.
Mike M