BREATHE BETTER,
LIVE BETTER
Many factors contributed to my development of this project. As a Physical Therapist, I have spent over 16 years in a large health care system. I am well aware of the impact of chronic disease. Chronic Obstructive Pulmonary Disease is one of the chronic diseases I have seen negatively impact a patient’s quality of life and put a financial strain on the health care system. I have often felt the skills of a Physical Therapist were underutilized with this patient population. It seemed that if more attention was given to development of specific interventions which addressed the primary limiting factor (dyspnea), then mobility would improve and length of stay would decrease. A win-win for all involved!
But the question for me was “How?”.
Was there evidence to support interventions beyond walking and limb strengthening
(the standard of treatment I had observed through the years)?
In EBP II, I researched this while searching to answer my PICO Question which asked if “Rib Cage Mobilizations or Incentive Spirometry” resulted in more significant functional outcome gains in persons with COPD.
The results of the literature search were disappointing. One thing which was confirmed was that incentive spirometry does not improve functional outcomes. However, support for rib cage mobilization to improve functional outcomes was not strong. In fact, though a good number of studies exist, the studies fail to use consistent treatment interventions, patients are of different severity levels and measurements of improvement were inconsistent. So, though studies exist supporting the benefit of improving chest wall mobility for dyspnea relief to improve functional mobility, the studies are of such poor quality that conclusive statements cannot be made.
CHECK OUT THE EVIDENCE TABLE FOR MY LITERATURE REVIEW: COPD Evidence Table
In follow up searching, more studies were located which supported mobilization(via stretching or manual therapy) of the rib cage for ease of breathing and rib cage expansion and other studies were located showing how improved rib cage expansion correlated to improved respiratory function measures and functional outcome measures. Unfortunately, the studies were not done together on the same subjects to bring it all together as a viable and necessary intervention. The information, however, was still useful and supported by the GOLD Standard (Global Initiative for Chronic Obstructive Lung Disease (www.goldcopd.com) recommendations for physical therapy interventions for persons with COPD.
 Limited mobility of RIB CAGE in person with COPD
Limited mobility of RIB CAGE in person with COPD
PURPOSE OF PROJECT:
The goal of my project was to bring this information to the attention of therapists who are treating patients with COPD in the hospital setting. I wanted Physical Therapists to see that they could add simple stretching exercises to the cardiovascular conditioning and strength exercises they are already doing and according to the literature, be able to improve function MORE than with walking and strengthening alone. I wanted the information to be IMMEDIATELY USEABLE and easy to understand to enhance the likelihood that practice standards would be altered as soon as possible, hopefully the afternoon following the in-service.
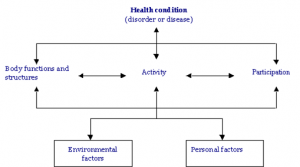
The presentation followed the logic of the ICF Model of Disablement which demonstrates how as a result of the MEDICAL CONDITION, PARTICIPATION (i.e. being a grandparent) can be negatively impacted due to ACTIVITY LIMITATIONS (i.e. can’t walk far) which result from IMPAIRMENTS (i.e. dyspnea related to lack of normal rib cage expansion).
THERAPISTS NEED TO DEVELOP INTERVENTIONS WHICH TARGET THE LIMITING IMPAIRMENTS TO HAVE THE GREATEST IMPACT ON RESTORING THE LIMITING ACTIVITIES WHICH IMPACT LIFE PARTICIPATION.
I developed the following to successfully share this information:
PRESENTATION FOR PHYSICAL THERAPISTS: A 45-minute presentation was created which provided the therapists in a rural hospital system the information needed to understand their role in the management of persons with COPD. Epidemiology of the surrounding area, the financial impact of COPD on their hospital, a brief pathology review and a review of the supporting literature was performed prior to reviewing the suggested exercises presented on the patient education handout.
Presentation: COPD Harnett Health inservice
Handout: Inservice worksheet
Feedback Summary from Physical Therapy department: Evaluation form COPD- summary
PATIENT EDUCATION HANDOUT: Exercises were developed based on reviewed studies and compiled into a patient education handout. Health literacy information was reviewed and utilized in the development of the hand out. Once complete, it was submitted to and approved by the Patient Education Committee at Harnett Health (Harnett County, NC) and was deemed in accordance with hospital standards for health literacy. The handout is currently being used in the Physical Therapy and Cardiac Rehab Departments at Harnett Health.
Patient Education Handout: Breathe Better Handout
EXAMPLE OF IMPACT OF THESE EXERCISES:
I did have a goal of adding a youtube.com site to the patient education materials, however, that media format is not yet supported by the Patient Education Committee at the hospital where I presented this information and though I feel it is a good start, I would like some professional advice and feel I will pursue this in the future. I did want to share with you the immediate impact these simple stretches can have. I performed a before video, did 8 minutes of stretches and then a follow-up video with a family member who has COPD and no other significant PMH. The difference is amazing! The only exercises she did are the ones you see pictures of, she held each for 10 seconds.
CHECK OUT THE PRESENTATION TO SEE THE BEFORE AND AFTER VIDEOS: COPD Harnett Health
I am hoping to be able to continue my interest in this area with my own actual study at Campbell University where I am an Assistant Professor in the Doctor of Physical Therapy program. I look forward to working with Dr. Doug Powell to develop baseline data on rib cage mobility and respiratory function and eventually bring in abnormal subjects, such as patients with COPD and other respiratory or rib cage dysfunction. I am excited to see the impact the profession of Physical Therapy can have on this chronic disease.
I want to thank you Dr. Doug Powell, Assistant Professor at Campbell University and Mrs. ALlison Bedsole, Director of Rehabilitation Services at Harnett Health for their assistance in completing this Capstone project.
REFERENCES:
1. Breunig IM, Shaya FT, Scharf SM. Delivering cost-effective care for COPD in the USA: Recent progress and current challenges. Expert Rev Pharmacoecon Outcomes Res. 2012;12(6):725-731. doi: 10.1586/erp.12.69; 10.1586/erp.12.69.
2. Fromer L, Cooper CB. A review of the GOLD guidelines for the diagnosis and treatment of patients with COPD. Int J Clin Pract. 2008;62(8):1219-1236.
3. Geddes EL, Reid WD, Crowe J, O’Brien K, Brooks D. Inspiratory muscle training in adults with chronic obstructive pulmonary disease: A systematic review. Respir Med. 2005;99(11):1440-1458. doi: 10.1016/j.rmed.2005.03.006.
4. Scherer TA, Spengler CM, Owassapian D, Imhof E, Boutellier U. Respiratory muscle endurance training in chronic obstructive pulmonary disease: Impact on exercise capacity, dyspnea, and quality of life. Am J Respir Crit Care Med. 2000;162(5):1709-1714. doi: 10.1164/ajrccm.162.5.9912026.
5. Zanotti E, Berardinelli P, Bizzarri C, et al. Osteopathic manipulative treatment effectiveness in severe chronic obstructive pulmonary disease: A pilot study. Complement Ther Med. 2012;20(1-2):16-22. doi: 10.1016/j.ctim.2011.10.008; 10.1016/j.ctim.2011.10.008.
6. Engel R, Vemulpad S. The role of spinal manipulation, soft-tissue therapy, and exercise in chronic obstructive pulmonary disease: A review of the literature and proposal of an anatomical explanation. J Altern Complement Med. 2011;17(9):797-801. doi: 10.1089/acm.2010.0517; 10.1089/acm.2010.0517.
7. Putt MT, Watson M, Seale H, Paratz JD. Muscle stretching technique increases vital capacity and range of motion in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2008;89(6):1103-1107. doi: 10.1016/j.apmr.2007.11.033; 10.1016/j.apmr.2007.11.033.
8. Malaguti C, Rondelli RR, de Souza LM, Domingues M, Dal Corso S. Reliability of chest wall mobility and its correlation with pulmonary function in patients with chronic obstructive pulmonary disease. Respir Care. 2009;54(12):1703-1711.
9. Leelarungrayub D, Pothongsunun P, Yankai A, Pratanaphon S. Acute clinical benefits of chest wall-stretching exercise on expired tidal volume, dyspnea and chest expansion in a patient with chronic obstructive pulmonary disease: A single case study. J Bodyw Mov Ther. 2009;13(4):338-343. doi: 10.1016/j.jbmt.2008.11.004; 10.1016/j.jbmt.2008.11.004.
10. Heneghan NR, Adab P, Balanos GM, Jordan RE. Manual therapy for chronic obstructive airways disease: A systematic review of current evidence. Man Ther. 2012;17(6):507-518. doi: 10.1016/j.math.2012.05.004; 10.1016/j.math.2012.05.004.




3 Responses to “COPD: Breathe Better, Live Better!”
Michael Tighe
Dear Michelle:
I absolutely LOVED the layout of your “Living with COPD” exercise patient handout!
How many times have we given patients reams and reams of documents with exercises, tips to avoid this or do that, cute little caricature drawings….and find it completely unread! No wonder the non-compliance rate with HEPs is so high!
It would have to be almost impossible to be non-compliant with this document!
Even the layout is designed for readability. Many years ago, I read a book about comic book and advertising copy layout, that described the way the human eye tends to scan written works: Our eyes start in the upper left hand corner, then drift down toward to page middle, out to the bottom left corner, then up and in toward the center, back down toward the lower right…continue this way around the entire page (imagine you are following the rough outline of a butterfly’s wings around the page!).
I thought this was a great project all around, BTW. To me, this is exactly what PT purports to be: an exercise-based modality, steeped in scientific background and biomechanical understanding, completely apart from a pharmacological base, highly reproducible, that improves independent function. Great job!
Michael Tighe
Michelle Green
Abby- Look for more research to come in this area in the future and thank you for your kind words.
Michelle
Abby Osborn
Michelle,
I was interested to read about your Capstone based on an anecdote you shared early on relating to a patient who really improved with some of these rib cage mobilizations and specific exercises in addition to typical acute care. And I am disappointed to see that your lit review didn’t show better evidence for this! No matter, I still think it is a great idea that I otherwise never would have thought of for trying out in the right scenario. Also, just general comments, you did a really impressive job with your exercise handout and powerpoint presentation. They were both very visually appealing and I think this is a skill/focus that will serve you well in your professor role at Campbell. Congrats, and good luck in continuing to get this info out there, I thoroughly enjoyed this site as well as your contributions online over the past year!
Abby